Understanding the Role of Surgery in Treating Metastatic Cancer
Metastatic cancer refers to the spread of tumor cells from the initial site into other parts of the body, making the treatment complicated. In most cases, systemic treatments, such as chemotherapy, are the mainstream of treatment. However, surgery is still an important modality in the management of selected cases of metastatic cancer. It may help improve the quality of life and, in selected cases, prolong survival.
Because of continuous development in medical technology, oncology surgery now gives new hope to patients with metastatic cancer. The article explains the various potential roles of surgery, including the relief of symptoms and the resection of metastatic lesions of the liver or peritoneum.
Why Surgery Matters in Metastatic Cancer
Surgery has been performed in selected metastatic cancers for strategic reasons. It reduces tumor burden and hence enhances the efficacy of systemic therapy, such as chemotherapy and immunotherapy. Sometimes, surgery is performed to resect solitary or a limited number of metastases with the intent to delay disease progression. For instance, surgical resection of liver metastases during the course of colon cancer has achieved impressive survival benefits.
Besides, the role of surgery in symptom management is indispensable: procedures that can relieve obstruction, stop bleeding, or decrease pain markedly are of utmost benefit in a patient's daily life. Surgery is rarely curative, yet usually forms a crucial part of a well-coordinated approach and thus is generally speaking advised under the direct care of a private oncologist.
Surgical Approaches Based on the Types of Metastatic Cancers
Patients with colon cancer liver metastasis are such those who can take liver resections, provided that disease extent has confined itself within the liver, allowing better survival with better outcomes once done with other systemic therapies.
Surgery for patients with metastatic pancreatic cancer remains much lesser since the time it would finally become useful may remain a choice more as palliative for such types of tumors when other symptom-causing diseases result.
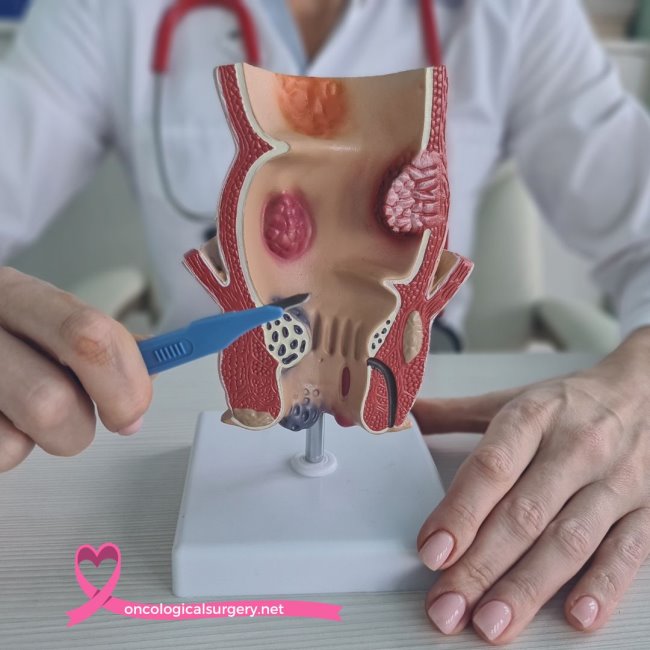
Gastrointestinal tract blockade resolution by a gastric and biliary bypass provides short-term but real relief among various gastrointestinal and also intra-abdominal tract neoplasias. Thus, HIPEC allows one to be even more radical in tumor elimination; hence, better post-procedure disease progression.
HIPEC stands for Hyperthermic Intraperitoneal Chemotherapy. Novel strategy but still performed in relation to surgery, where heated chemotherapy is given right into the abdomen immediately following the surgical procedure of removing all visible tumors. Such an approach targets those tiny cancer cells which can't be removed by surgery.
HIPEC really finds its indication in diseases such as peritoneal carcinomatosis and in the advanced treatment of stomach cancer. This method, when used together with surgery, often results in better overall survival and low recurrence rates among the patients.
Surgical Benefits in the Treatment of Metastatic Cancer
Surgery by itself may not be curative for the metastatic condition of cancer. Yet it has significant symptomatic benefits. A decrease in the size of a tumor enhances the effectiveness of other treatments for the cancer and, in some instances, delays disease progression. That is so when metastases are solitary and surgery can result in long-term remission.
Palliative surgery avoids suffering through pain or dysfunction of organs. Surgical intervention may make life more bearable for such patients, which underlines the necessity of a multidisciplinary treatment approach, considering surgical options at any time.
Limitations and Considerations
By no means does every metastatic cancer patient consider surgery a better option. There is a need to be very cautious with the extent of the disease, the overall state of the patient's health, and associated risks. Hence, it could be that the extent of metastasis is too great or serious co-morbid states exist; therefore, non-surgical methods may be more indicated.
Secondly, surgery is always difficult after one has gotten weakened by previous treatments. A discussion with one's oncologist will help make an informed decision based on needs-that is, whether to go through it, considering the risk versus the benefit involved.
Modern Surgical Techniques
Surgery for metastatic cancer has been made to be much safer and effective. The modern surgical modalities that include laparoscopic and robotic-assisted surgeries have reduced recovery times and complications. Such advancement allows for very accurate tumor removal while preserving healthy surrounding tissues.
Introduction of technological advances, such as intraoperative imaging, the accurate detection and targeting of metastases by the surgeon are greatly enhanced. These are very helpful in complicated cases arising during certain treatments, such as bile duct cancer, in improving surgical outcomes and enhancing the recovery experience of patients.
Combining Surgery with Systemic Therapies
Surgery is more effective for many metastatic cancers if done with systemic treatments such as chemotherapy, immunotherapy, or targeted therapies. In such a situation, this modality of treatment will be comprehensive in both the primary tumor and the distant metastases. For instance, those patients undergoing HIPEC often have better outcomes if systemic therapies are included in their treatment plan.
Such interventions act in synergy with surgery by improving survival and reducing recurrences. Consultation with a multidisciplinary medical team is very important in optimizing the treatment strategy for optimum outcomes.
Surgery represents one of the many facets in the treatment of metastatic cancer; it may be therapeutic or palliative in nature. Although not for every case, when applied appropriately, surgery has impressively changed the face of survival and quality of life. Technological development, along with further refinement in techniques, continues to expand the horizon, thus making surgery assume a very important place in current oncology practice.
It is always highly recommended to consult a private oncologist if you or your loved one were considering treatments. Be it colon cancer treatment or assessing the advantages of surgery for colon cancer liver metastasis, a personalized approach always works in the best interest of the patient in the battle against metastatic cancer.