Phone
+90 532 203 7931Thyroid cancer is a type of cancer whereby cancer cells proliferate in thyroid gland tissue. The thyroid gland is a butterfly-shaped gland located in the base of the neck, below the larynx. It plays a very essential function in the regulation of so many body functions such as heartbeat, pressure, body temperature, and metabolism through regulation by the released hormones. There exist four major cancers that make up thyroid cancer: papillary, follicular, medullary, and anaplastic. They all differ in features and, as such, in the way they should be treated. They also differ in outlook.
Thyroid cancers, however, need diagnosis and categorization so that therapy can be chosen accordingly. The most prevalent is papillary thyroid cancer with favorable prognosis. Less prevalent than papillary type but with generally good prognosis is follicular thyroid cancer. Parafollicular cells, the thyroid 'C' cells, give rise to the medullary thyroid cancer. The most rare but most dangerous is the anaplastic thyroid cancer; in some cases, this is treated with aggressive therapy. These are all decisions that need to be made so that the doctor can devise proper treatment on a patient-by-patient basis.
Symptoms and Diagnosis
Understanding the Signs
Early thyroid cancer is asymptomatic in most cases. When and if it becomes symptomatic, the following is noted: lump, most likely in the neck, palpated in the skin; this, with time, enlarges and, in very rare cases, becomes tender. Occasionally, there is voice change or chronic hoarseness in the tumor having affected the vocal cords.
The second set of symptoms that is found with advanced thyroid cancer is difficulty in swallowing and fullness in the neck. It is also accompanied by pain in the neck and the throat. Enlarged lymph nodes in the neck would be a sign that cancer already spread in the nearby lymphatic tissue. All these symptoms point towards the necessity for early detection and regular check-ups, especially in individuals most susceptible to thyroid cancer. Thyroid cancer can happen at any age.
Diagnostic Techniques:
The Diagnosis is made by a sequence of tests and procedures in thyroid cancer in Turkey. There is palpation of the neck, for instance, for lump and thyroid deviation. Blood tests would help in detecting the level of thyroid hormone in the body. In a few cases, thyroid markers such as thyroglobulin would be detected that would lead towards cancer. Scanning by ultrasonography is typically done in thyroid and detection of cancerous nodules.
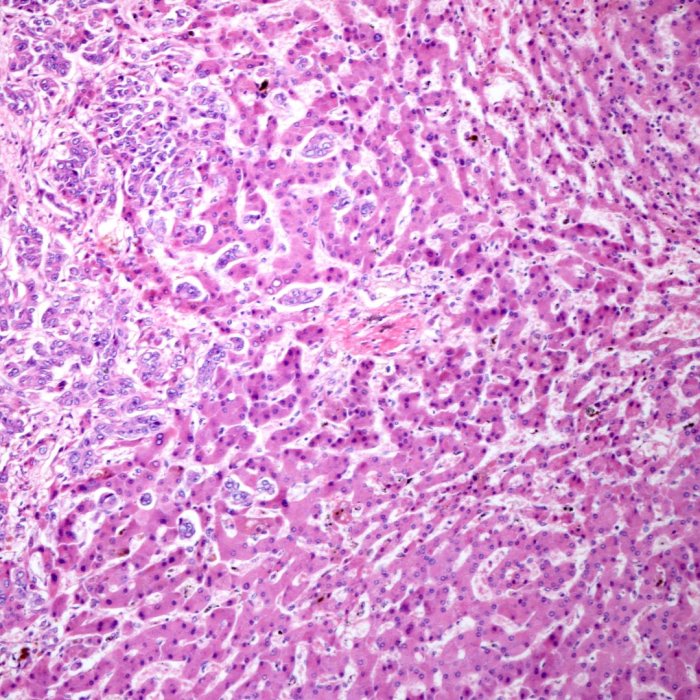
Fine needle aspiration biopsy (FNAB) is a procedure in which cells from the thyroid nodule are extracted with a very narrow needle. They are thereafter examined with a microscope to determine whether the cancer is benign or malignant. Additional imaging studies, like radioactive iodine scan, computed tomography (CT) scan, magnetic resonance imaging (MRI), or positron-emission tomography (PET) scan of the body, can reveal cancer size and whether cancer is spread in remote areas of the body. These tests will be very useful in determining the best treatment.
Treatment Options
Operation
The primary treatment for thyroid cancer in most cases is surgery. The aim is excision of the tumor and/or excision of the whole or a portion of the thyroid gland. The nature and type of surgery would be depending on the type and stage of cancer. Total thyroidectomy is excision of the whole thyroid gland and lobectomy is excision of a portion of the gland. In cases of lymph node spread of cancer, lymph node dissection would be necessary.
However, surgery is much less traumatic, with lesser damage and also with smaller wounds today. With such a surgery, one's risk for recovery and complications after surgery can be minimized. Infection, bleeding, and injury to the parathyroid glands and laryngeal nerves are the complications. Properly planned post-operative care and observation will certainly control and minimize such complications for uneventful recovery.
Radioactive Iodine Treatment
The patient must also swallow a capsule, and liquid radioactive iodine, during radiation iodine therapy in order to destroy any leftover thyroid tissue, as well as cancer cells, after surgery. The therapy is successful, especially in papillary and follicular thyroid cancer, since thyroid cancers absorb iodine. The thyroid cells would be destroyed by the radioactive iodine, but that level of damage would be done by it in any other type of tissue.
It is also tolerated well, with side effects occurring in very few individuals. The most common side effects include metallic taste, dry mouth, pain or soreness in the neck, and malaise. Side effects in severity are mild and transitory. Patients treated with radioactive iodine can be made aware about some dietary limitation as well as about some safety precautions so that radiation exposure in others in their surroundings is minimal.
Outside Radiation Therapy
The radiation is administered from outside the body, in which it kills the cancer cells by utilizing beams of radiation. It is applied in most cases in advanced thyroid cancers, or in cases in which surgery and treatment with radioactive iodine is not possible. It is helpful in symptomatic control with better tumor control.
New techniques, such as intensity-modulated radiation therapy, allow irradiation with very precise sparing of the normal tissues. The most frequent radiation therapy side effects include skin reaction, fatigue, and dysphagia. These should be treated appropriately so that the patient does not lose his quality of life throughout his course.
Chemotherapy
Chemotherapy: Treatment with drugs that kill cancer cells or stop them from growing. It is rarely applied in treating most thyroid cancers but, in treating advanced, aggressive anaplastic thyroid cancer, sometimes it is. It is taken by mouth or injected intravenously.
The most commonly prescribed chemotherapy drugs for thyroid cancer include cisplatin and doxorubicin. Side-effects that can be experienced include vomiting, nausea, hair loss, and susceptibility to infection. Chemotherapy is most typically administered in combination with additional treatment, as the treatment alone would be unlikely to be effective and the disease would be uncontrolled.
Targeted Therapy
Targeted therapy is achieved through drugs that target the molecules that participate in tumor creation and tumor enlargement. The therapies and drugs possess the capability to stop the tumor cells from growing and proliferating and do nothing, if anything, to the body's normal cells. Two such targeted therapies with widespread application in thyroid cancer treatments include sorafenib and lenvatinib; the drugs belong to a category of tyrosine kinase inhibitors.
The second target that would be specific in gene mutations would be through the employment of RET inhibitors such as selpercatinib and pralsetinib. All target drugs would be less likely to produce any side effects than in the traditional chemotherapy method. But their efficacy would be tumor-specific depending on the genetic setup, and treatment regimens from case to case would be in place.
Hormone Therapy
After surgery, in which the whole or portion of the thyroid gland is removed, thyroid hormone replacement is required so that the metabolism is balanced, as well as so that any cancer cells that can be left behind would not be restored. It is achieved by taking man-made thyroid hormone in the form of medication like levothyroxine, by mouth, daily. Hormone replacement is very important so that overall health and well-being is preserved.
It requires regular check-up of the thyroid hormone level and adjustment in the dose according to the level. It enables the patient to enjoy a healthy and balanced lifestyle with proper regulation in the replacement therapy for the hormone. The patient should strictly comply with the treatment and inform the practitioner about the problem.
Support and Living
Nutritional Support
The recovery and healing process would be assisted by nutritious food during thyroid cancer treatment. A balanced diet with whole grains, lean proteins, fruits, and vegetables would maintain strength and energy. Hydration would be maintained by consuming more fluids.
Avoidance of iodine, especially before radioactive iodine therapy, would be advised by some. A nutritionist would be consulted in order to plan a customized meal plan, in consideration with individual requirements and eating habits. Follow-up visits, held at regular periods, can steer a patient through various nutritional traps and can prove rewarding in the long term for the patient.
Counseling Psychology
The cancer is emotionally and psychologically exhausting. Emotional and psychological support is strongly required in the areas of stress, depression, and anxiety about the disease. The patients make use of various support services that extend from support groups, therapy, and counseling. Professional therapy and counseling also provide support and coping skills, while support groups balance the lack of professional training with survivor community familiarity and support.In addition, most support from friends and family can provide additional reasons for a patient to be in better psychological health.
Lastly, mind-body treatments such as meditation, yoga, and mindfulness also tend to lower stress and provide help with improved psychological health.
Advancements in Clinical Trials When thyroid cancer is treated, it is through clinical trials that treatments for thyroid cancer are created by experimenting with the new treatments and adjusting the existing treatments. In this way, a patient is treated with better treatments that cannot be accessed by all. It is through this study that the clinicians and researchers obtain information about the disease and treatments. There is a purpose behind all these phases of clinical trials. Safety and proper dose is verified by Phase I trials for a novel treatment. Phase II trials determine whether a treatment works and what the adverse effects would be. Comparison with the existing treatments in relation to relative efficacy is made in Phase III trials.
Long-term impact and safety after it is approved is overseen in Phase IV trials. Patients seeking clinical trials should consult with their health care team about the possible benefits and harms. Hope in the future Thyroid cancer is a dynamic subject matter; there are novel approaches with promise in the future.
Gene therapy with genetic repair of mutations associated with thyroid cancer leads to person-specific treatment regimen. Personalized medicine is focused on individualization of treatment according to the genetic background and nature of tumor in the individual in such a way that the treatment is efficient and fitting. Combinations of more than one type of treatment also increasingly are being studied in their attempt to optimize their efficacy. These developments, through continued study and testing, allow thyroid cancer individuals to be provided with the best obtainable survival rate and quality of life. Knowledge about the most current studies and treatments provides the patient, as well as family members, empowerment with the information so that they can make important decisions in their treatment. There has been a substantial enhancement in thyroid cancer management, and it is well-known for having a full range of care. Early detection, individualized treatment plan, and full supportive treatment rank among the things that one would desire in this fight against thyroid cancer. The patient and his/her family members are encouraged to seek information, support, and employ all means of available treatments that can be utilized in order to maximize their chances to defeat the disease.