Phone
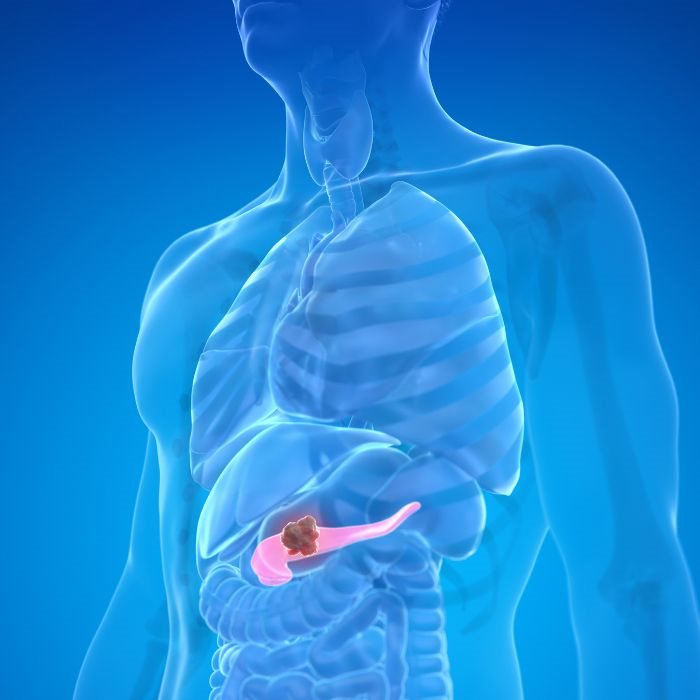
+90 532 203 7931One of the most critical modalities of treatment regarding the staging, diagnosis, and excision of the tumor and cancerous tissues is oncological or cancer surgery in Turkey. It is a critical part of the treatment of cancer and involves various procedures all triggered by one cause-to remove the cancerous cells and prevent the spread of the disease. The following is the type of oncological surgery, how the process is done, how the recovery is made, and the news within this specialty.
The Role of Oncological Surgery in Cancer Treatment
Surgery is the vital part of the cancer treating process. Oncological surgery can either be curative with the intention of eradicating all the cancerous tissue or symptomatic, or palliative care with the aim of improving the quality of life in a cancer patient. Having the role of oncological surgery helps the patient and his relatives decide the right option for their therapeutic alternatives since the quality of life and survival are directly associated with the interventions offered by surgery in Turkey.
Most cancers are first treated with surgery. For the localised type of tumor, the removal of the tumor through surgery can be a cure when combined with other approaches such as chemotherapy and radiation. When the cancer is not so amenable to treatment, surgery may ease symptoms and pain and thus produce a longer and more tolerable life. Surgery may assume many different functions in the treatment of cancer depending upon the specifics in the individual case. It is thus frequently the focal point of overall cancer treatment.
Types of Oncological Surgery:
Diagnostic Surgery
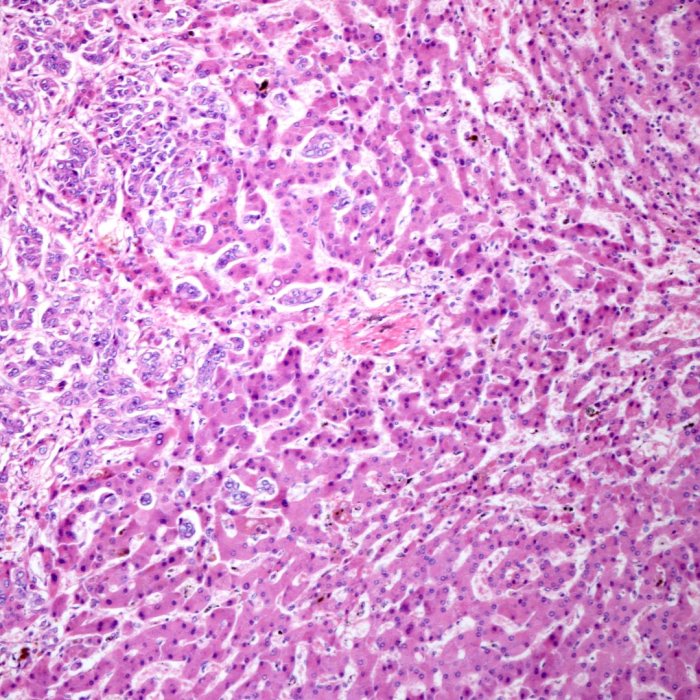
Diagnostic surgery provides a sample of the tissue upon which a biopsy can be performed and assists with diagnosing and staging the cancer. Endoscopy and biopsy are diagnostic surgery. A biopsy is the surgical excision of a sample of the tissue for microscopic examination. A biopsy is needle biopsy, incision biopsy, and excision biopsy based upon the site and the nature of the tumor.
These are the processes in which a thin tube with a camera is inserted into the body in order to visualize internal organs or remove tissue samples. The minimally invasive processes enable physicians to diagnose the cancer without having to make large incisions, thus minimizing the recovery time and complications. Diagnostic surgery is an entrance into a cancer experience; thus, diagnostic surgery provides very critical information that assists the treatment process.
Restorative Surgery
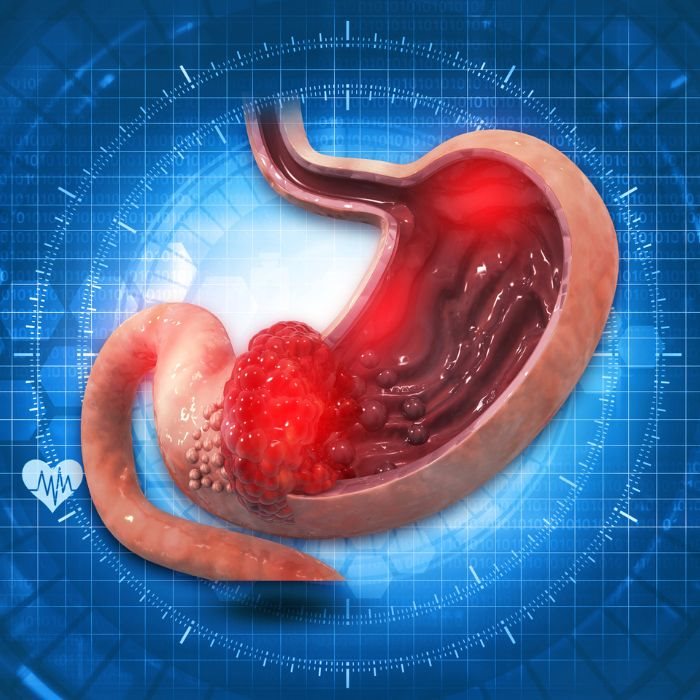
Curative surgery involves the removal of the entire tumor and some surrounding tissue with the goal of curing the individual. Obviously, this kind of surgery is optimally done when the cancer is detected early and not yet spread into other tissues. Some examples of curative operations are lumpectomy, mastectomy, colectomy, and prostatectomy. With a lumpectomy, the surgeon excises the tumor and a minor amount of surrounding normal tissue; this is most typically performed when treating breast cancer. Mastectomy involves the removal of either one or two breasts and is used for advanced breast cancer.
Colectomy is the partial or total removal of the colon as a treatment for cancer of the colon. Prostatectomy is the partial or complete removal of the prostate gland and most frequently occurs as a treatment for cancer of the prostate gland. The operations are used with the goal of removing the cancer from the body. Further therapies usually follow with the goal of destroying whatever cancer cells are left. Curative surgery has also turned very precise and efficient with the advancement of the surgical method.
Debulking Surgery
In the event that the entire tumor cannot be eliminated, debulking surgery is performed with the goal of removing as much as is practicable. It is performed with the goal of improving the effectiveness of other treatment modalities, such as chemotherapy or radiation therapy. It is most frequently performed for ovarian cancer because the masses are usually large and spread into the surrounding tissues. Reducing the tumor burden through surgery usually alleviates symptoms and therefore improves quality of life.
This operation is one of the very strong arguments for multidisciplinary cancer care: surgical care plus other care may be necessary for control of the disease. It shows how surgical care can be modified for different phases within the natural evolution of the cancer, alleviating symptoms and enhancing survival where cure is not feasible.
Palliative surgery
Palliative surgery is not performed with the intent for the removal or cure of cancer but for symptom relief and quality-of-life improvement. The most appropriate time for palliative surgery is with advanced cancer patients when the goal for treatment shifts from the control or removal of the disease to symptom control and comfort. Examples are the placement of a stent for airway or vascular patency and the placement of a gastrostomy tube for nutrition where the oral route cannot be used.
This palliative surgery improves the quality of life for these patients regardless of the diagnosis through the alleviation of some symptoms. It is yet another critical humane component of cancer care with focus towards comfort and quality improvement of the patient and not merely the eradication of the disease.
Reconstruction Surgery
Reconstruction surgery is also done for the restoring the body part where cancer surgery was done back to its original function and looks. Surgery is generally needed when a lot of tissue loss occurs during cancer treatment. Mastectomy with subsequent breast reconstruction and reconstruction following head and neck cancer surgery are two good examples. Two ways the breast can be reconstructed are with the aid of implants or with the usage of the tissue from a different site.
Reconstruction surgery of the face can be caused by removal of cancerous tumor from the head and neck region to ensure the structure and function of the region. The reconstruction procedures also promote psychological well-being such that the individual feels normal and gains back their confidence.
Preventive or Prophyl Surgery
Preventive surgery refers to the surgical removal of tissue from the body with a strong potential for developing cancer before the cancer develops. It is a preventable approach where one would otherwise carry a significantly higher risk than the others for certain cancers perhaps because of issues with genes or other causative factors. Prophylactic mastectomy and prophylactic oophorectomy are some examples. Prophylactic mastectomy involves the surgical removal of breasts either one or two for the risk reduction of breast cancer. Prophylactic oophorectomy involves the removal of ovaries surgically for the risk reduction of ovarian cancer.
It is also called preventive because it involves the removal of vulnerable tissue. Preventive surgery can significantly decrease the incidence of cancer within the body. Preventive surgery is a recent coming together of genetics, family medical history, and surgery within the cancer treatment options and allows a high-risk patient the ability to be pro-active with their medical care.
Surgical Procedures
Open surgery
In open surgery, the major incision is given with the intention of revealing the tumor and surrounding tissue. The classical approach does allow good visualization of the site but with the disadvantage of longer recovery time and higher risks for complications. However, the majority of the cancers must receive open surgery for good visualization with respect to vision and accessibility for removal.
Yes, it is admittedly extremely successful for treating a wide variety of cancerous diseases. Although it is invasive, doctors have mastered the process with the least amount of side effects and complications and thus make it reliable for treating millions of patients.
Minimally Invasive Procedure
Minimally invasive surgery involves minimal cuts and thereby promotes quicker recovery and fewer complications. Some procedures involve the use of a thin tube with a camera called a laparoscope through which visualization and removal of the tumors with minimal cuts are made, and robotically assisted surgery where robotically powered mechanisms under the guidance of the surgeon allow precise, minimally invasive operations.
These developments have transformed the oncological surgery and benefited the patients with reduced pain, shorter stay in the hospital, and faster return towards normal life. Minimally invasive procedures are a leap quantum ahead of treatment through surgery because they are technologically advanced instruments combined with quality surgical expertise.
Laser Surgery
Laser surgery involves intense beams of light used for cutting or eliminating tumors. The most common sites where laser surgery is used are skin cancers, cervical cancers, and other cancers accessible by laser. It causes the minimal amount of damage to surrounding healthy tissue and may be done with little pain.
Laser surgery is a valuable asset in the armamentarium for the surgeon due to the precision with which very early cancers and premalignant lesions can be handled. The recovery is immediate without involving the invasion into the body, making it perfect for appropriate candidates.
Cryosurgery
Cryosurgery involves the actual freezing of the tumor cells with the help of liquid nitrogen or argon gas with the intention of destroying the cell completely. It is employed for the initial stages of skin cancer and precancerous lesions. It is a minor process and can be done as an outpatient. It is a highly effective modality for the treatment of such type cancers.
Success with the removal of local cancer through the use of cryosurgery reflects the role for it in current oncological surgery. Cryosurgery is a high-reward/low-risk cancer treatment with little damage caused to the tissues within a tumor bed and with the cancerous cells killed.
Electrosurgery
Electros Electrosurgery is a surgical method involving high-rate electrical currents which are capable of cutting and destroying the cancer cells. It is employed where oral cancer and skin cancer are operated. The end outcome is the removal of the tumor exactly with minimal blood loss through the surgeon's capability to remove the cancer cells entirely.
Precision and accuracy provided by electrosurgery make it the cornerstone of current day cancers. Clean margins are attained with the aid of the use of electric currents with fewer recurrence risks.
Mohs surgery
Mohs is very precise as a skin cancer treatment. The skin is removed layer by layer and immediately microscopically inspected for cancer cells until no cancer cells are found. Thus, the cancer is completely removed with the maximum amount of normal tissue preserved.
Moh's surgery is a painstaking process aimed at minimizing the scarring on the patient and ensuring the maximum possibility of a favorable outcome. It is really the epitome of precision and attention, towards which every contemporary oncologic surgery aspires, and most significantly, cosmetically focused neoplasms.
Recovery and Rehabilitation
Postoperative Care
Recovery from oncologic surgery varies with the size and extent of the surgery. Prevention of pain and infection and monitoring for complications are the most prominent. Prevention of pain and control through medication and technique are extremely vital elements of recovery comfort.
Another major component of this is wound care: the wound site must remain clean and draped to aid healing. After complications-bloody, infectious issues, etc.-the wound must be closely monitored very closely to ensure any issue can be attended to in time and the ease with which the healing process sets in.
Physical Rehabilitation
This rehabilitation can help the patient identify his functions and strength after the operation. This might include physical therapy exercises aimed towards gaining mobility and strength so the person can get back into daily activities earlier. Occupational therapy can also help one learn the basic daily activities which will help with independent functioning.
Rehabilitation is a very crucial stage of the healing process with physical and functional dimensions. Working with rehabilitation experts can generate the best results in recovery and increase the quality of life.
Psychological and Emotional Support
Emotional and psychological effects need to be managed after cancer surgery. Counseling and therapy support services help patients deal with depression and anxiety as well as other related emotional issues occurring during and after treatment. Support groups help provide a sense of community and commonality and make patients not feel alone.
Psychological and emotional support are needed as part of complete cancer care. Depression or anxiety caused by the invasion of cancer into their lives can be avoided during this time through professional mental care. It is one of the means through which care providers indicate their concern for the healing of their patients from the invasion of cancer into their lives. It also helps them deal with complications caused by the setback.
Follow-Up Care
Follow-up visits are essential for tracking recovery and recurrence. It may involve physical examination, imaging studies, and laboratory tests which may be required to remain cancer-free. It also provides the opportunity for the control of any ongoing symptoms or late effects and counsels patients on continuing care around the clock on an individual basis.
Follow-up regular visits place the care provider team and the patient continuously on the lookout for the first signs of recurrence and thus give them reassurance about favorable results in the long term.
Evolution in Oncological Surgery
Personalised Surgery
Personalised surgery here would imply tailoring the surgery to the individual patient based upon the molecular and genetic makeup of the person's cancer. What this would imply is better targeting of the cancer tissue with the prospect for better results. Personalised surgery is intended to capitalise upon such advances in molecular diagnostics and genetics testing to tailor treatment to the individual patient.
This aligns with the trend towards precision medicine in oncology where the treatment is tailored according to the individual characteristics of the patient for the respective cancer. Focusing the emphasis on the individual functioning helps the clinicians intervene better with better outcomes.
Intraoperative imaging
Intraoperative imaging Intra-operative modalities are computer tomography and MRI scans that produce images during the operating process in real time. The modalities will thus facilitate the surgeon's ability to identify the tumor with precision and excise it with precision and thus perform better surgery. The surgeon gets the whole perspective of the operating site with the aid of intra-operative imaging and thus can make appropriate intra-operative judgments.
This is one of the recent critical innovations in surgical technique, involving precision and minimizing the possibility of tumor left behind. One of the good examples of enhanced surgical outcome and protection for the patient through the aid of technology is intraoperative imaging.
Minimally Invasive Techniques.
New minimally invasive technologies are constantly evolving that further enhance surgical technique with the concomitant improvement in the outcome for patients. They decrease the recovery time for patients and minimize complications. Developments in the evolution of laparoscopy and robot-assisted surgery have expanded the spectrum of cancers amenable to minimally invasion.
As these methods improve over time, the physicians are now able to carry out safer and more effective options for the patients that enable faster recovery and general good health. Among the present leaders in the area of advanced surgery are minimally invasive procedures, which are revolutionizing cancer treatment and the prognosis for the patients.
Immunotherapy and Surgery
One of the recent approaches, and one with great potential, is combining immunotherapy with surgery. The immunotherapy assists the body's immune function in destroying the cancer cells, otherwise the radical surgery would be superfluous. The inclusion of immunotherapies with surgery assists the medical experts in helping the body's normal defense against the cancer cells, thereby facilitating better therapies.
This combination therapy thus reflects the synergy between the two modalities of cancer treatment based upon the strength of the respective modalities. Indeed, the search for new means by which the two modalities may be combined pushes the limits of possibility for the treatment of cancer.
Lastly Although surgery very often provides hope to many patients and even cures their cancerous disease, the future is not bleak with the continuing advancement of surgical technique and instruments. The future appears auspicious because study and development are ever-progressing in the field of oncologic surgery. This enhances the overall approach toward cancer handling and changes the overall picture of the process.