Phone
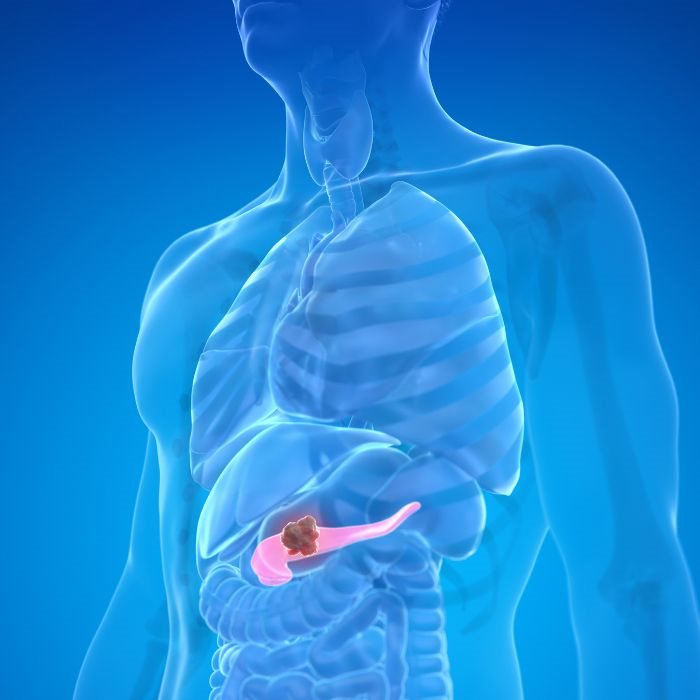
+90 532 203 7931Pancreatic cancer is a very aggressive and multifaceted tumor that occurs in the gland located behind the stomach but is a critical contributor in digestion and control over blood sugar. Due to its location and role, pancreatic cancer is typically diagnosed very late, by which point early symptoms are very non-specific, so it is one of the most difficult cancers to treat.
Early detection is crucial.
It is critical that the disease is diagnosed early so that the course of the disease can be made favorable. Unfortunately, pancreatic cancer is very difficult to diagnose early since it has nonspecific and insidious symptoms. The initial symptoms can be so nonspecific that they might be confused with less dangerous diseases, with the result that the diagnosis is made in an advanced stage. When diagnosis is made, after the disease is in advanced stages and is difficult to treat, the chances for efficient treatment become fewer.
In spite of such hurdles, much can be done to maximize the chance for early detection. For example, awareness about risk factors such as family background, smoking, chronic pancreatitis, and specific genetic mutations can lead to increased and earlier screening in individuals with increased risk. Advances in imaging technology, in addition to awareness that specific tests can look for individual disease markers in the blood, can lead to earlier detection in the future-in the possibility that the disease is more susceptible at that point.
Diagnosis and Symptoms
Pancreatic cancer is detected at earliest, if at all, after the onset of symptoms. Symptoms in pancreatic cancer would generally be non-specific depending upon the size and location of the tumor, and also depending on whether the tumor is spread in any area in the rest of the body. Some of the general symptoms of this cancer include jaundice, yellowing of eyes and skin, weight loss, which is involuntary, abdominal pain with pain radiating in the back, loss of appetite, vomiting, and onset of diabetes. These symptoms would generally be nonspecific and would be caused by numerous disorders, and diagnosis is rendered very difficult accordingly.
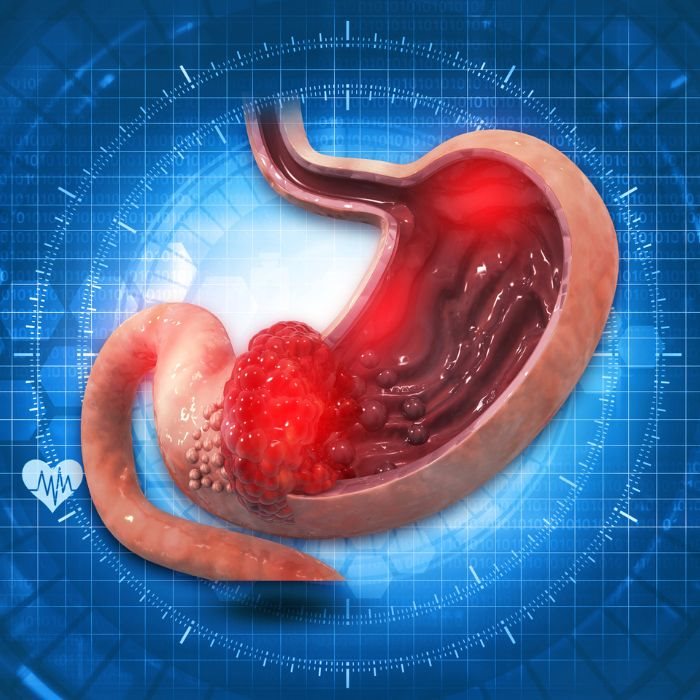
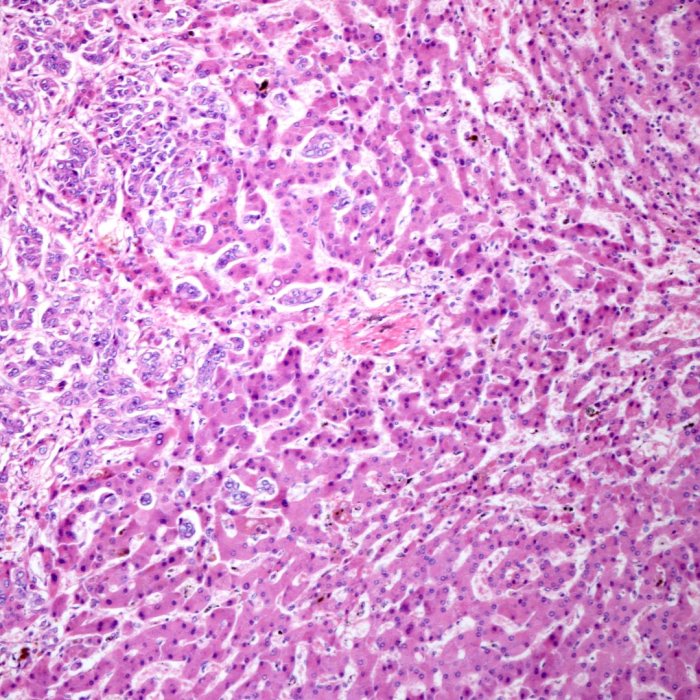
Pancreatic cancer is diagnosed most frequently by the use of imaging tests, studies in the bloodstream, and testing by biopsy. These imaging tests-the CT scan, MRI, and PET scan-provide images in detail of the pancreas and surrounding organs in order to assess tumors and spread. Fine-needle aspiration, through the scope, and endoscopic ultrasounds all utilize the endoscope with internal ultrasonography probe in order to obtain precise images, and fine-needle aspiration can be done through the scope in order to obtain samples. Blood testing for tumor markers such as CA 19-9 is helpful, but one cannot be diagnosed with pancreatic cancer through testing in the bloodstream. A biopsy is most frequently required, in which a sample is looked at with a microscope in order to assess for cancer cells.
Treatment Options
The treatment of pancreatic cancer is determined by cancer stage, overall health, and patient preference. Treatment can range from surgery, radiation, chemotherapy, target therapy, and immunotherapy. Surgery is still the main treatment in the situation in which cancer is localized and can be removed. The most common surgery is that in which the head of the pancreas, portion of the intestine, removal of the gallbladder, and portion of the bile duct is excised. Other surgical procedures that can be done include distal pancreatectomy and pancreatectomy, depending on tumor location.
Radiation therapy: It is a type of treatment that utilizes beams with high energy in order to destroy cancer cells by targeting them. It is applied pre-operatively in order to shrink tumors, is applied post-operatively in order to destroy the cancer cells that remain, or for the relief of symptoms in advanced cancer. More recent approaches such as EBRT, SBRT, and IMRT minimize damage to normal tissues. It can be given as chemotherapy-a systemic treatment with drugs that destroy the cancer cells or prevent their progression-and can be neoadjuvant, adjuvant, or palliative.
Targeted Therapy
Targeted therapy is a more recent type of cancer therapy designed with specific molecules that play important roles in forming and developing cancer cells. They function by targeting in order to prevent cancer cells from growing and multiplying with fewer detrimental effects on normal cells. Erlotinib (Tarceva) targets the epidermal growth factor receptor (EGFR) and is paired with gemcitabine for cancer that has spread in the pancreas. Olaparib (Lynparza) is a class of drugs that is referred to as PARP inhibitors. A patient with a mutation in their BRCA1, or BRCA2, gene would be treated with this drug. Fewer side effects would typically be expected with these newer target treatments than with more traditional, older chemotherapies; however, many genetic complications as well as usual complications of the tumor itself can impact efficacy.
It is more recent and works by using the body's own defense against cancer. It does utilize drugs that must be injected that help the body recognize and destroy the cancer cells. It is in the testing phase but is also proving effective in treating pancreatic cancer. The drugs, such as pembrolizumab (Keytruda) and nivolumab (Opdivo), that act as checkpoint drugs stop proteins from occurring in cancer cells that prevent the immune response. Immunotherapy vaccines that activate the body's defense against specific antigens hold promise and are being studied.
Support and Lifestyle
Diet plays a very strong role in treating pancreatic cancer and general health. Proper diet could ease symptoms, support the immune system, and make one feel generally better. Foods that were more calorie-rich and contained more proteins fight weight loss and wasting muscles, and eating moderate portions frequently is best tolerated and can avoid nausea and loss of appetite. Only if a patient is lacking in getting enzymes from their pancreas naturally would pancreatic enzyme supplements be required.
A consultation with a registered dietitian would be the best nutritional assistance during the treatment period. Pancreatic cancer is typically linked with depression, anxiety, and stress support cares. Coping skills are achieved through learning from experienced psychologists and counselors, and they provide psychological support. Support groups provide inspiration and support through the assistance of people undergoing the same.
The patient is also assisted by strong support networks consisting of friends and family members; the support group provides psychological support and practical assistance. Mind-body techniques involve meditation, yoga, and mindfulness that help with stress relief and psychological resilience.
Advantages in Research
Clinical trials provide the means through which new treatments and interventions from previous ones take place. They provide the patient with the advantages of accessing novel treatments as well as provide physicians with the opportunity for gaining more information about illness. In trials in Phase I, what is safe and in what period the treatment would be given is determined. In trials in Phase II, how efficacious a treatment is and further monitoring of the side effect is continued. Whereas in Phase III trials, treatments are compared with the standard treatments, in Phase IV trials, long-term side effects of the acceptable treatments are being observed. It is essentially in clinical trials that treatments become accessible in some before they become generally available, but the volunteerism is full of risks.
The pursuit of better management or treatment for pancreatic cancer goes on. Researchers are investigating some of the most promising upcoming approaches, such as gene therapy, in which genetic mutations that cause pancreatic cancer are attacked with specially designed therapies, and personalized medicine, in which therapy is individualized according to the patient's genetic blueprint and tumor profile. Treatment approaches in which more than one treatment approach works in harmony in order to treat the disease are being investigated.
Indeed, such developments enhanced pancreatic cancer patient survival and quality of life. Pancreatic cancer is a deadly cancer; but with continued study and advancement in more efficient treatments, the disease is less formidable. Early detection, individualized treatment, and full support is the key in fighting this cancer. It is strongly advised that patient and family should be well educated about the disease, treatment, and receive any assistance and support that can be offered.