Phone
+90 532 203 7931What is HIPEC, and how is it applied?
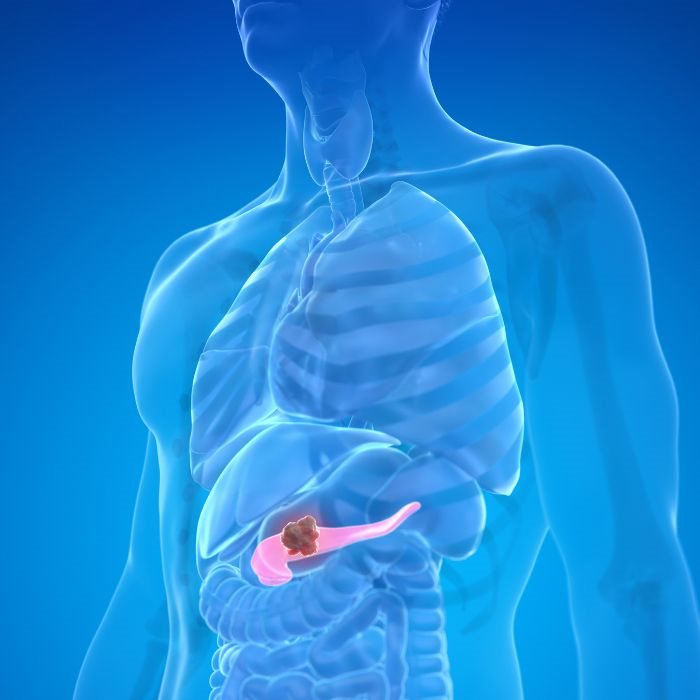
HIPEC is a novel approach to the management of intra-abdominal cancers, including but not limited to peritoneal carcinomatosis, ovarian cancer, and selected cases of colorectal cancer. The route of medication administration for HIPEC is unlike any other mode of chemotherapy drug administration; almost all chemotherapies are given intravenously, whereas this route delivers warm chemotherapy directly into the abdomen. It is therefore prudent that this approach will allow the administration of higher concentrations right at the place where the cancerous cells are present, hence assurance of better results in treatment with minimal systemic side effects.
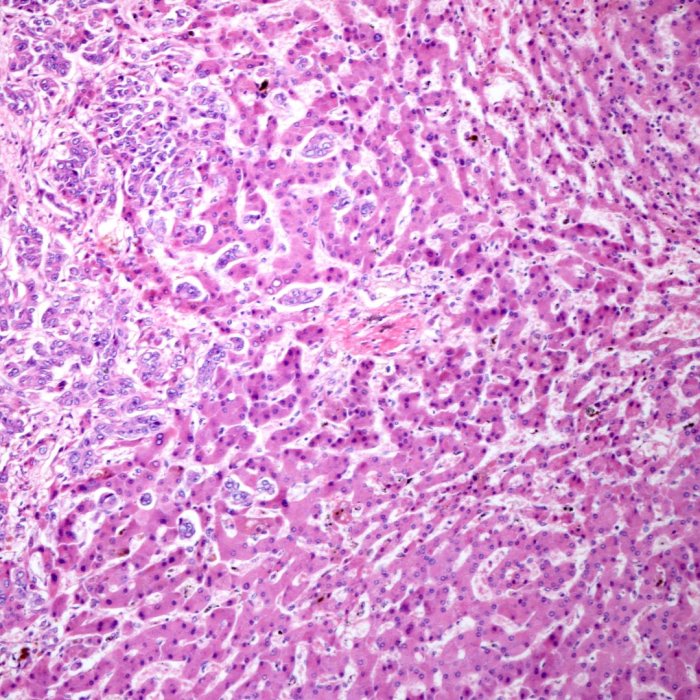
HIPEC is usually performed right after cytoreductive surgery, which is the physical removal of a tumor that can be seen. Following surgery, a heated chemotherapy solution is circulated through the intra-abdominal cavity for about 60 to 90 minutes. The heat increases the absorption of the chemotherapy by the tumor cells, making the treatment more effective. The solution is drained off from the body at the end of treatment, and the incision is closed.
It is for this reason that this modality of surgery, together with HIPEC, forms a strong one-two punch against cancers of the abdomen-whether they be primary or recurrences-paving fresh hope for those whose former treatment options have been limited.
Indications for HIPEC
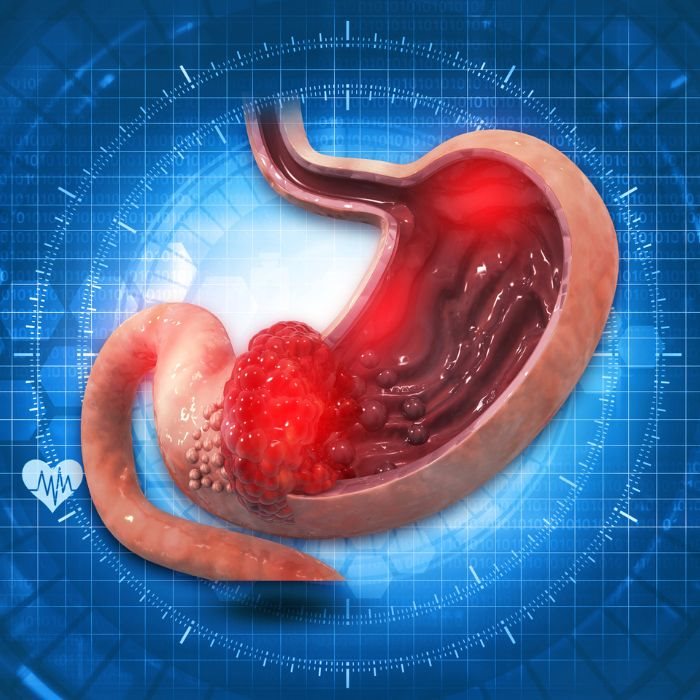
Conditions most associated with HIPEC are those cancers that have spread within the peritoneal cavity itself but that have failed to metastasize to more distant organs. The typical examples include peritoneal carcinomatosis, pseudomyxoma peritonei, mesothelioma, and certain manifestations of ovarian and colorectal cancers. It is most effective in cases where the cancer is confined within the abdominal cavity and can be reduced surgically to a minimum tumor burden before the application of chemotherapy.
Most patients consider HIPEC when they have few alternatives with conventional therapy. HIPEC thus becomes very helpful in conditions whereby standard chemotherapy and radiation have failed to control the disease. This decision is thus undertaken after very careful evaluation by a multidisciplinary team that includes surgical oncologists, medical oncologists, and radiologists who evaluate overall patient health, his disease extent, and the possible benefits of the procedure.
Alternative Treatments to HIPEC
While HIPEC is certainly a one-of-a-kind approach to a variety of cancers involving the abdomen, there are several other treatments that can be considered as alternatives under appropriate conditions, taking into consideration both the actual status of the disease at hand and the overall health status of the patient. Classical systemic chemotherapy remains the standard for most tumor types when these have already extended beyond the peritoneal cavity. Radiation therapy can be indicated, more so for localized control of tumor growth.
Other options include targeted therapy, which employs medicines designed to fight specific cancerous cells based on their genetic or molecular profile. Then, of course, there is immunotherapy-it uses the body's immune system against cancerous invaders, mostly for patients carrying specific genetic markers, hence making them candidates for such treatments. Even then, HIPEC often represents a more localized, effective treatment option in comparison for such patients with peritoneal carcinomatosis and other similar conditions.
Benefits and Risks of HIPEC
Therefore, the key benefit of HIPEC is that the high concentration of chemotherapy affects tumor surfaces in the abdominal cavity while limiting it to the rest of the body. The treatment of this nature, since it is localized, would enhance the killing of cancerous cells and reduction of tumor size by chemotherapy, thereby improving survival and the quality of life in patients of advanced cancers of the abdomen.
As with all medical treatments, however, there are risks with HIPEC as well. Possible complications include infection, bleeding, and injury to surrounding organs from major surgery in conjunction with heated chemotherapy. Patients can develop side effects related to the chemotherapy itself, which may include nausea, vomiting, and temporary hair loss. The treatment's possible risks and benefits should be discussed by the patient with the medical team to determine if HIPEC is right for them.
Preparation for HIPEC
Preparation toward HIPEC is multidimensional: from extensive general health assessment and imaging studies regarding tumoral burden to even biopsy for confirmation. Blood work and cardiac evaluation may also be part of a preoperative workup in selected patients to show proper physical fitness for surgery.
Preparation Most the patients will be put on a special diet some days before the surgery and are supposed to go through bowel preparation to clean their intestines from food remnants. Such preparations diminish the risk of complications during the operation and give greater access to the abdominal cavity to the surgeon. The patient also needs to report to the doctor about the medications taken, because a part of them will be changed or stopped for some time before the procedure.
During the HIPEC Procedure
Cytoreductive surgery involves the initial steps of the HIPEC procedure, where the surgeon removes the maximum amount of tumor visible in the abdominal cavity. It is an integral part of every HIPEC procedure where the focus is given to reducing tumor burdens prior to the application of chemotherapy. It is a major surgery that may take a number of hours depending on the number and size of the tumors.
After the surgical resection, the HIPEC treatment may be initiated. It entails the heated chemotherapy solution, generally at 42 to 43 degrees centigrade, circulating all over the abdominal cavity with the help of a special pump. The chemotherapy is then allowed to "bathe" for 60 to 90 minutes to allow any remaining microscopic cancer cells to come out to be exposed to the treatment.When the chemotherapy has been drained, the surgical team closes the incision and moves the patient to a recovery area where close monitoring may be carried out.
Postoperative Care after HIPEC and Recovery
Recovery from HIPEC is often protracted and cumbersome, adding the risk of major surgical complications to the chemotherapy effects. Thus, a protracted stay in the hospital-usually for several days-is quite essential to observe any signs and complications, such as infection, bleeding, and even organ dysfunction. Basic supportive care therefore includes pain management, nutritional support, and physical therapy aimed at regaining strength and mobilization in the early postoperative period. The period of recuperation at home for each patient differs; most of the patients are allowed to rest for few weeks and are advised to avoid lifting heavy weights and doing strenuous activities.
Follow-up visits with the medical care provider are recommended regarding further monitoring of the recovery process, side effects, and the response of the treatment. Further imaging studies will be needed after some time in order to determine if the cancer has recurred.
Follow-up and Long-term Outcomes
One important attribute of care after HIPEC is long-term follow-up. Patients will be expected to return for routine follow-up care with their oncology team; this is to be carried out in a manner similar to other oncology patients, with routine physical examinations, blood tests, and imaging studies in search of any evidence of recurrence. The frequency of such visits will be related to the individual patient's condition and the treatment plan in general. Other follow-up care aside from recurrence includes management of long-term side effects brought on by the surgery and chemotherapy. Nutritional needs can be considered, and pain or discomfort managed along with other facets of support, enabling the patients to be mentally equipped to deal with the problems associated with recovery. The emphasis is to make sure that patients not only survive but thrive after their treatment with the best quality of life possible.