Phone
+90 532 203 7931Colon Cancer
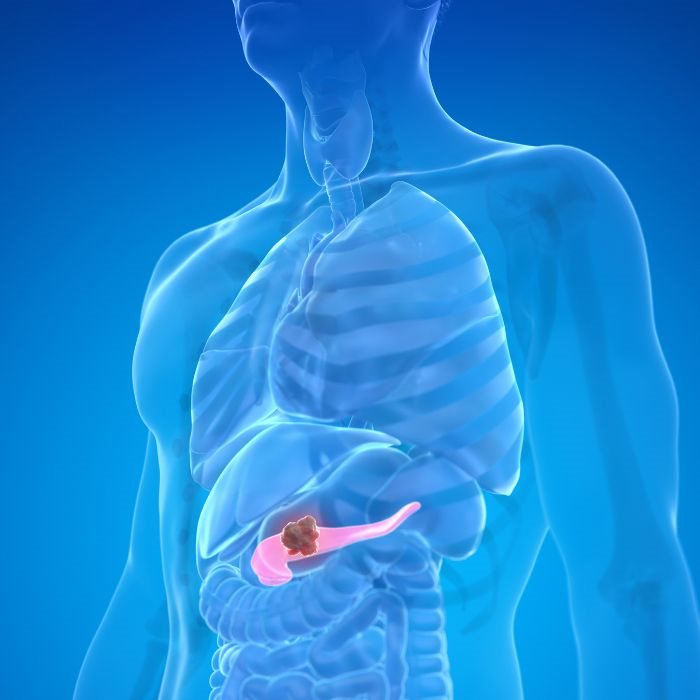
It is sometimes called colon cancer, though it is actually a certain type of cancer that begins either in the large intestine or the rectum, which are the last parts of the digestive tract. Being among the most common cancers in the world, it thus affects millions of people each year. Most colon cancers begin as noncancerous growths, or polyps, in the lining of the colon and gradually develop into malignancies. While the survival rate is very good among patients with an early-stage diagnosis of colon cancer, which is treatable by surgery, the situation is quite different and grim when the disease advances.
In more advanced stages, the cancer of the colon would have metastasized to other parts of the body, such as the liver. The metastatic growth of tumors will, therefore, occur once the liver is reached by the cells originating in the colon. The process dictates that the disease has reached an advanced-and-intractable stage. Hepatic metastases of colorectal origin by themselves, therefore, affect prognosis and demand a complex and interdisciplinary style of treatment.
The prognosis of colon cancer spread to the liver had historically been unfavorable, and only variable possibilities for symptomatic palliation were offered, many with symptomatic benefits but extension neither of the patient's quality nor quantity of life. Rapid improvement in surgical techniques, liver-directed therapies, and personalized cancer treatments has re-awakened optimism for this disease entity. Undoubtedly, patients with liver metastases from colon cancer can seek a variety of modes of treatment nowadays that will improve not only their survival chances but also offer them a better quality of life.
Our Center is deeply committed to providing the most advanced, the most recent, and most effective treatments. We strongly believe that appropriate combinations of therapies could enable even impossible accomplishments in olden days to achieve for patients whose cancer of the colon had spread to the liver. It is the deeply devoted team's unparalleled hard work that brings customized care to each patient according to his or her case and opens a window of hope again in the treatment of this horribly devastating disease.
Therapy of colon cancer has radically changed in the last decades, especially in cases where liver metastases develop. Previously, liver metastases were a sign of the terminal stage of the disease, where basically nothing much could be done except what one calls palliation. Emphasis was put basically on symptomatic management, which also included, when possible, improvement of the quality of life for a short period of time. However, with the new treatment modalities available in today's medical science, patients are now experiencing a new lease of life and an enhanced survival time.
Surgical Resection: The Cornerstone of Treatment
It remains one of the most effective modalities in cases of colon cancer metastasis to the liver, especially if it has been localized to a particular area of the liver. Surgical removal of the tumor and the consequent tissue affected by the tumor is now available to more patients due to the improvement in surgical techniques and is far safer. In fact, the invention of laparoscopic and robotic-assisted surgeries really changed the face of liver resections as regards recovery time, reduction of complications, and better overall outcomes. Surgical resection decisions are made depending on the size and number and location of liver metastases but also on the general condition and liver function of the patient. Surgery can ensure long-term survival and a possible cure in some cases for a patient with limited and resectable liver metastases.
Our surgical services work in close consultation with the treating medical oncologist, radiologist, and other related specialists to determine the appropriate modality for each of our patients, thereby assuring totally rigorous yet caring surgery.
Surgical resection doesn't necessarily need to be just a removal of the cancer, though. In many patients in whom the disease is such that they can undergo complete resection, very significant improvements in survival are realized. The disease-free interval for some patients is measured in years, and for some, it is permanent remission. Our surgical team does a lot of hard work in trying to maximize that potential for each individual patient to give them that best chance of long-term survival.
Liver-Directed Therapies: Targeting the Metastases Directly
When resection is impossible, liver-directed therapies offer alternative ways of treating patients. These modalities represent several techniques for the effective targeting of liver metastases. Liver-directed therapies specifically target the liver to kill the cancer cells or cut off their blood supply. Some common liver-directed therapies include:
Radiofrequency Ablation (RFA)
This technique employs high-energy radio waves that ultimately cause heating and destruction of the cancer cells. RFA is usually indicated in patients with smaller or fewer metastases that are not amenable to surgical removal. It is minimally invasive and sometimes percutaneous-that is, through the skin-which makes it quite appealing to the patients with limited metastases.
Transarterial Chemoembolization (TACE)
This is a combination of chemotherapy and embolization: the process by which the blood vessels supplying a tumor are blocked. Because TACE delivers chemotherapy to the liver tumor locally and then cuts off the blood supply afterward, it is very good at shrinking tumors and controlling their growth. This modality of treatment comes in handy for those patients who have larger or diffuse metastases which can't be surgically removed.
Stereotactic Body Radiotherapy (SBRT)
It has been recognized that SBRT is a form of radiation therapy in which very large doses of radiation are given to small areas of the liver with very good targeting. This will ensure minimum damage to the healthy tissue surrounding the area and maximum effect on the tumor. Often used in patients with inoperable metastases, SBRT can be used alone or for complementation to other kinds of treatment.
These liver-directed therapies are performed at our center in a very precise manner with great care, backed by advanced technological interventions and expertise. A fully integrated, multidisciplinary team carefully evaluates each patient's condition to determine the appropriate therapy or therapies. Since these treatments are directed against the liver, they are better positioned to accomplish noticeable tumor control and symptoms reduction, which would in turn improve the quality of life and add to the overall extended survival times.
Systemic Chemotherapy and Targeted Therapies: Attacking Cancer Throughout the Body
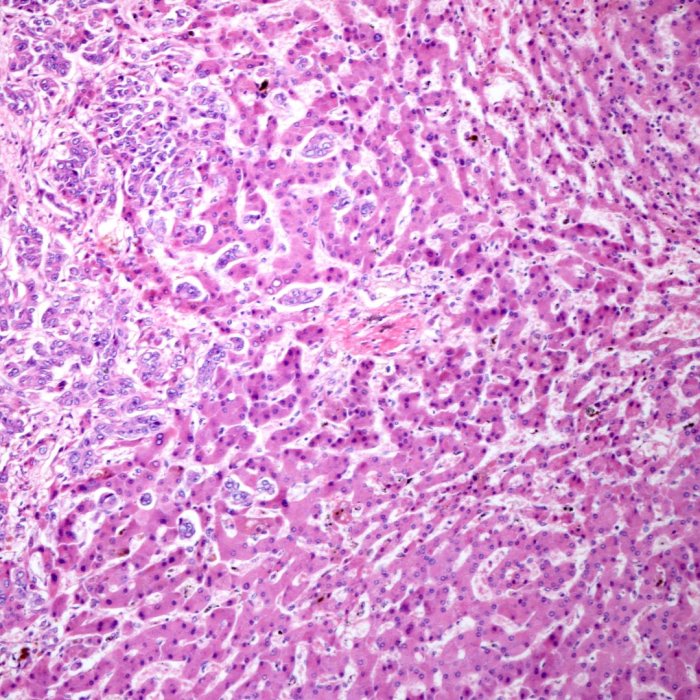
Systemic chemotherapy conventionally formed the backbone of the treatment for advanced colon cancer, especially when involvement of the liver took place. Chemotherapy will, therefore, have to be instituted in every patient with diffuse metastasis since it attacks the cells of the cancer. Improvement in chemotherapy regimens in the recent past and the evolution of targeted therapies have made a big difference in the outcomes of patients suffering from colon cancer with liver metastases.
Targeted Therapies
These agents inactivate or kill tumor cells depending on their genetic and molecular profiles. For instance, monoclonal antibodies shut down some proteins involved in the growth of the tumor cell; other types of targeted therapies could affect the capability of the tumor to repair DNA, establish new blood vessels, or perform other vital functions. These types of targeted therapies could be used concurrently with chemotherapy; this treatment would increase the lethality of the therapy and decrease its impact on normal cells.
With every development that takes place within the fields of oncology, we redo our strategy and try to provide nothing but the best and the latest to the patients. By personalizing this chemotherapy regimen in accordance with characteristics of the patient and his tumor and genetic pattern, we actually manage to enhance the efficacy of the treatment while reducing the adverse effects to a bare minimum.
In that way, we prolong the period of existence and improve life conditions of the patients in whom colon cancer is diagnosed at more advanced stages. Immunotherapy is one of the newest, really exciting developments in treating cancers that, for selected patients carrying particular genetic profiles, including those with high microsatellite instability-such as MSI-H or mismatch repair deficiency, dMMR-is broadening. It works in sharp contrast to conventional therapies attacking the cancerous cells directly by raising the body's immune system against cancer cells more effectively.
Immune checkpoint inhibitors are medicines that turn off proteins that get in the way of the immune system's ability to fight against cancer cells. Moreover, these checkpoint inhibitors also block the function of 'checkpoint' molecules to free a person's immune system to attack the cancer, a completely new avenue of treatment for patients with advanced colon cancer. The various clinical trials and research projects in which our center is involved are aimed at proving the role of immunotherapy in patients with liver metastases from colon cancer and offering new potential hope for those patients qualifying for this particular approach when other treatments have been exhausted.
The essence of such efforts is the integration of immunotherapy into our treatment schemes, which renders our patients eligible for the latest developments within oncology and opens partially important avenues towards improved survival.
The Need For Multidisciplinary Care
Succinctly, successful management of liver metastases from colorectal cancer requires a system whereby experts of the relevant specialties are pulled together to consider a management strategy for the individual patient. Because of this, at our center, a team comprising the big four disciplines-surgery, medical oncology, radiation oncology, and interventional radiology-is assembled in a comprehensive treatment package for the patient. It will ensure that this strategy considers the disease process right from the principal tumor in the colon down to the metastatic lesions in the liver.
We meet regularly as a team to discuss the cases of each of our patients to find the most appropriate and all-inclusive treatment modalities. Such teamwork shall hence facilitate the delivery of continuous and coordinated care experiences, where each specialist in his field shall add a piece toward the best possible outcomes. It is by this multidisciplinary approach that we are hopeful of taking treatment and therefore hope to our patients.