Phone
+90 532 203 7931Mark's Journey to Recovery
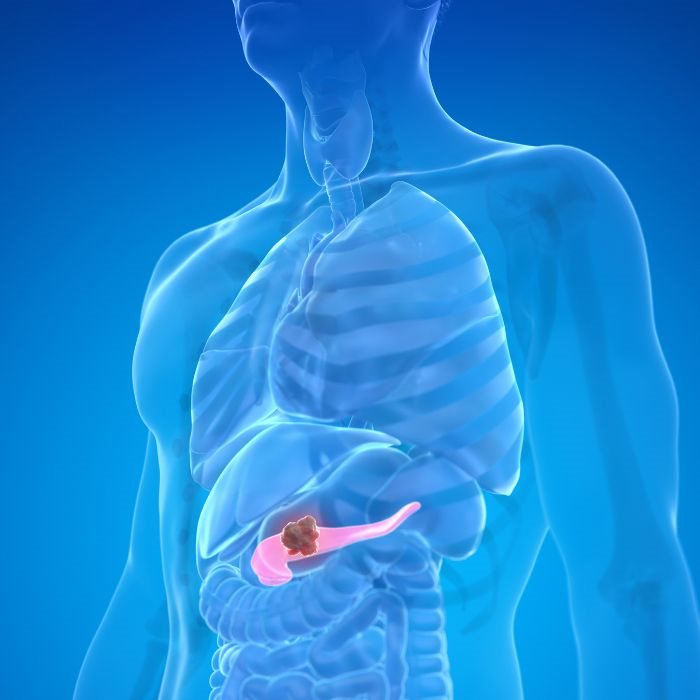
Mark is a 63-year-old engineer with pancreatic cancer. It was a huge surprise when he was diagnosed, and the circumstances presented in a grim manner. The tumor is large and embroiled in the vital blood vessels close to his pancreas. The initial consultations indicated that surgery may not be possible because the tumor was too complex in its involvement with the superior mesenteric vein and portal vein. However, through a second opinion, Mark became aware of advancements in surgery, such as vascular reconstructions and shunt surgeries, that would keep his life supported.
Mark underwent a complex surgical procedure in which the surgical team performed a vascular reconstruction, removing the tumor and reconstructing the blood vessels affected by the process. Restoration of normal blood flow led to successful resection of the tumor. Mark underwent a long recovery but succeeded and stands today as a living example of innovative surgical intervention in rallying to the challenge that vascular involvement has brought about with respect to pancreatic cancer.
The story of Mark is indicative of how advanced procedures such as vascular reconstructions and shunt surgeries are now acting to expand the horizons of pancreatic cancer surgery from what was until recently considered to be unresectable disease and, therefore, without hope of curative surgery.
Vascular Reconstructions in Pancreatic Cancer Operations
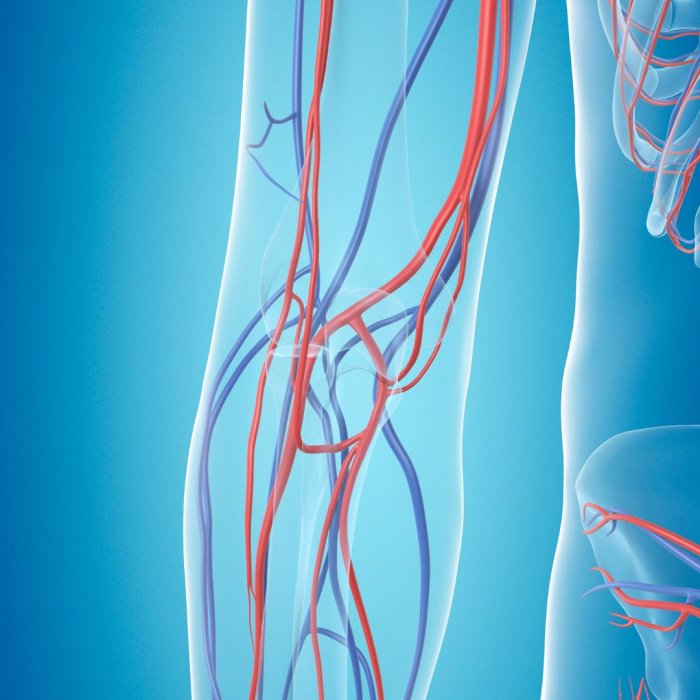
Vascular reconstructions have acquired major significance in the surgical management of pancreatic cancer, particularly when the tumor invades locally or encases major blood vessels. The pancreas is related to a number of important vessels, such as the SMA, SMV, portal vein, and celiac axis. If a tumor extends into these vessels, further management with standard surgery may not be possible unless vascular involvement has been addressed beforehand.
The aim of vascular reconstructions is the resection (removal) of an affected portion of a blood vessel followed by reconstruction through direct anastomosis (reconnection) or by graft. This is particularly important whereby a tumor cannot be removed without removing the segment of the vessel it has invaded.
One common scenario is involvement of the SMV or portal vein. In such cases, the affected portion of the vein is resected with the tumor, and the vein is reconstructed to ensure normal blood flow. This reconstruction, if needed, can be performed with a vein graft from another part of the body or by using a synthetic graft.
Vascular reconstructions have greatly changed the definition of what is considered resectable in pancreatic cancer. In the past, unresectable pancreatic tumors were thought to be those involving major blood vessels. With the availability of vascular reconstructions, many of these tumors can already be operated on, providing these patients a good chance for long-term survival.
Shunt Surgery: Redirection of Blood Flow to Enable Resection
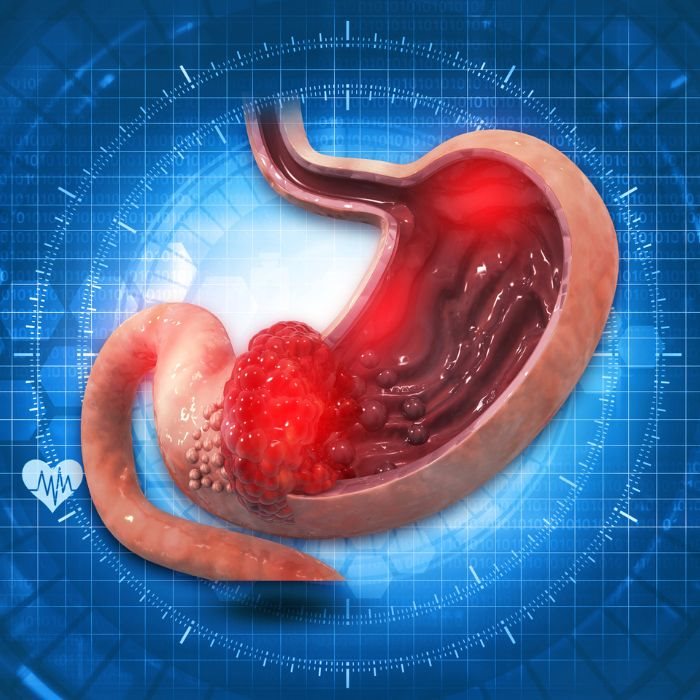
Shunt surgery is another new methodology that is again very central to the treatment of pancreatic cancer with vascular involvement. The shunts are utilized basically for the re-routing of blood flow from one area of the body to another part, avoiding the blockage or the site of involvement of the disease. In the case of pancreatic cancer, shunt surgery would rely on this procedure only if tumor involvement with the blood vessels makes simple excursion or reconstruction of the vessel unattainable.
Shunt surgeries for pancreatic cancer: The most commonly performed shunt surgery for pancreatic cancer is portosystemic shunting. This surgery is specially used, in case of tumor manifestation on the portal vein, where in other terms its surgical resection will have serious disruption of the blood flow, making this difficult.
Shunting thus allows the possibility to actually bypass the affected area so that the tumor can safely be resected and cancerous tissue removed without any mishap in the circulation of blood. Shunt surgery can also be incremented with yet an additional way for vascular reconstruction, useful in most complex cases, thereby contributing to the armamentarium for management of advanced pancreatic cancer.
Vascular Resection Techniques And Their Overcoming Of The Complexities Of Vascular Involvement by Advanced Methods
Perhaps the most challenging aspects of pancreatic cancer surgery are vasculature involvement. The intensive blood supply to this organ renders surgical intervention very risky, particularly when the tumor has already invaded or encased such vessels. Recent advances in techniques, including vascular reconstructions and shunt surgeries, have opened new doors to treatment.
These are highly specialized surgical techniques that mandate not only a high level of surgical expertise but require involving physicians from multiple disciplines, often calling for collaboration between pancreatic surgeons, vascular surgeons, and interventional radiologists. Preoperative planning is very crucial and often involves detailed imaging studies, including CT angiography or MRI, which help delineate the relation of the tumor with surrounding vessels.
In certain situations, neoadjuvant therapy achieves tumor downsizing, with a subsequent decrease in the degree of vascular involvement. In patients with locally advanced pancreatic cancer, the integration of neoadjuvant therapy with advanced surgical interventions resulted in an improvement in prognosis.
Innovations in Vascular Reconstruction and Shunting Surgery
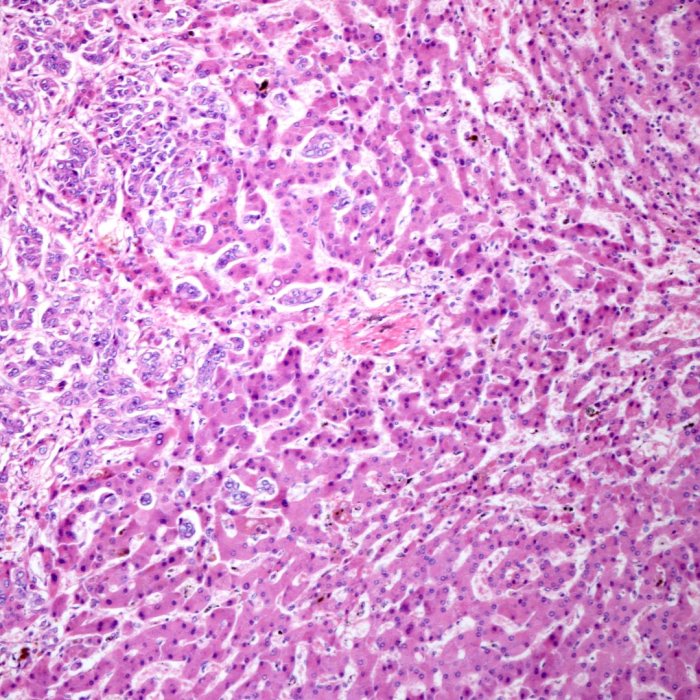
The discipline of vascular surgery is inundated with a lot of advanced inventions, which are directly putting an impact on the treatment of pancreatic cancer. The use of advanced imaging technologies, such as intraoperative ultrasound and 3D imaging, permits detailed visualization of the clarity of the tumor and surrounding vessels and necessitates precise and effective resections of such tumors.
Along with this, graft development using new materials—be it synthetic or bioengineered—has shown giant advancements, thereby improving the overall success rates of vascular reconstruction. These are biocompatible and hardy materials, hence reducing the risks attached to various complications like that of graft failure or infections.
Shunt surgery has therefore been carried out more easily through minimally invasive procedures such as laparoscopic or robot-assisted shunt surgery; these techniques have been responsible for reducing the recovery times further while improving the chances of recovery. Relative to more invasive surgeries, the implantation of shunts through minimally invasive approaches results in the accurate placement of shunts with less destruction of the surrounding tissues, hence a very appealing option for patients who are not candidates for more invasive surgery.
Impact on Patient Outcomes: Extending Survival and Quality of Life
Vascular reconstructions and shunt surgeries have become invaluable; they tilt the scales of outcomes for patients and, further, obviously alter the landscape in the field of the treatment of pancreatic cancer. All this has led to better survival rates in patients and, in many situations, gives the patient a real chance of long-term remission.
Research has shown that patients who undergo vascular reconstructions in combination with removal of tumors have the greatest survival potential compared with purely non-surgical treatments. This especially holds for surgical teams that are specialized in high-volume centers in pancreatic cancer.
The improved survival, of course, is supported by the advanced surgical techniques. Procedures that may manage the involvement of vessels will reduce symptoms of pain and problems with the intestines, so the patients can lead as near-normal lives as possible during and after treatment.
Rebuilding Hope with Vascular Reconstructions and Shunt Surgery
The challenges posed by vascular involvement in pancreatic cancer are immense, but the development of new advanced surgical techniques that include vascular reconstructions and shunt surgeries is now bringing new hope to patients. These procedures are now stretching the frontiers for surgical intervention that will enable clear margins even with resections of hitherto-reverted-unresectable pans and most importantly bring in positive survival and quality of life.
For a patient like Mark, whose cancer was directly tied to critical blood vessels, these advancements have offered new hope—a road to recovery that seemed shut before. As surgical techniques advance and our understanding of pancreatic cancer becomes ever deeper, the future of treatment becomes increasingly hopeful, with yet more options available for even the most complex cases.