Phone
+90 532 203 7931A Patient's Story: Sarah's Unexpected Battle
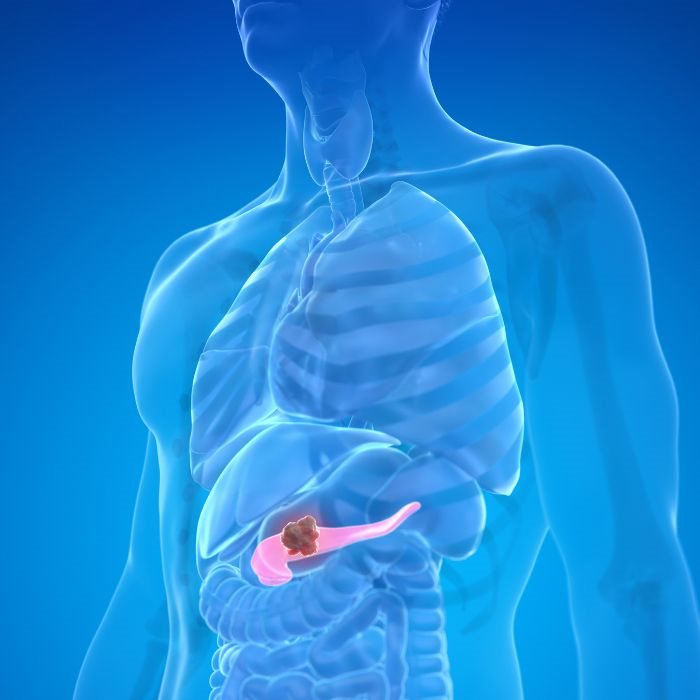
Fifty-two years old, mother of two, and proud of being healthy, Sarah found herself suffering from chronic abdominal pain and losing weight without any intention. This was quite far from being major health issues for her; at first, she just wrote it off as stress. But the case worsened, and going to the doctor proved it. After a battery of tests, Sarah was diagnosed with pancreatic cancer, a disease that was about to change her life. However, her fight would not be an easy one. Doctors in Lancaster discovered that it was a locally advanced tumor, having infiltrated other nearby structures, including the superior mesenteric vein and portal vein, which made her treatment a whole lot more complex. The vascular invasion of the mass made her case in an already very challenging case all the more complex to treat.
What is more, though, is that Sarah is the exception. Pancreatic cancer is one of the most aggressive of all cancers, noted for the invasion of its surrounding blood vessels, adding another layer of obscurity that could make treatment very onerous. The purpose of this paper is to clarify what pancreatic cancer is, discuss what vascular invasion is, and explain how this complication raises significant barriers for treatment.
What is pancreatic cancer?
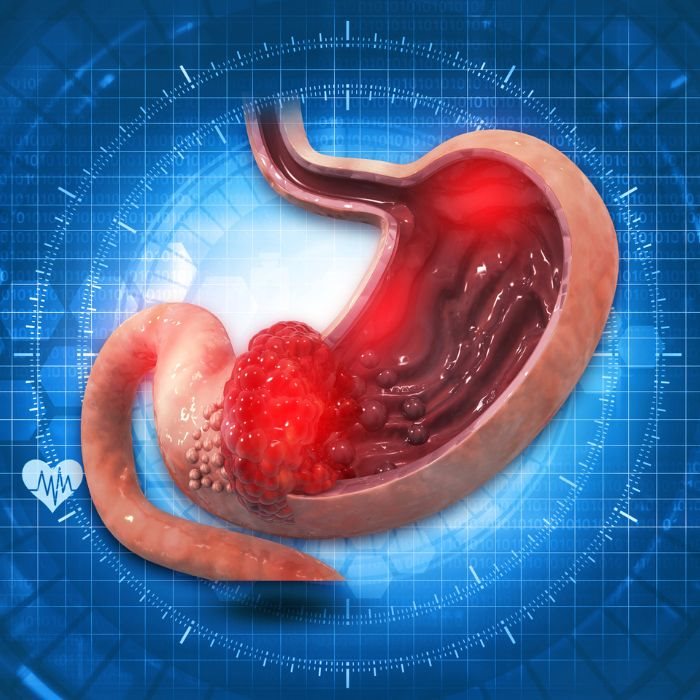
It begins in the pancreatic cells, which are a tissue of an organ placed behind the stomach. The pancreas helps in digestion of food and blood sugar control. The pancreas' two significant cells are one is the exocrine cells which made up digestive formed enzymes, and the other has the endocrine cells, which are involved in the creation of many hormones that include insulin. Most pancreatic cancers are from the exocrine cells and are known as pancreatic adenocarcinomas.
This kind of cancer is highly insidious, as it may remain asymptomatic until it reaches its advanced stage. This usually is when the cancer is already at an extended level and could have spread to other organs by the time its symptoms, such as jaundice, abdominal pain, or weight loss, are manifested. One of the reasons pancreatic cancer has a very poor prognosis, with less than a 10% five-year survival rate, is approximately due to the growth of the cancer without symptoms.
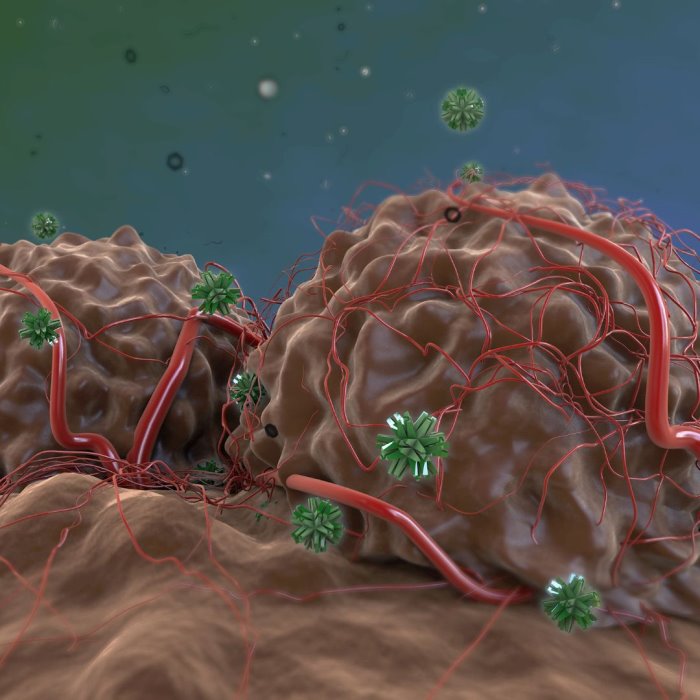
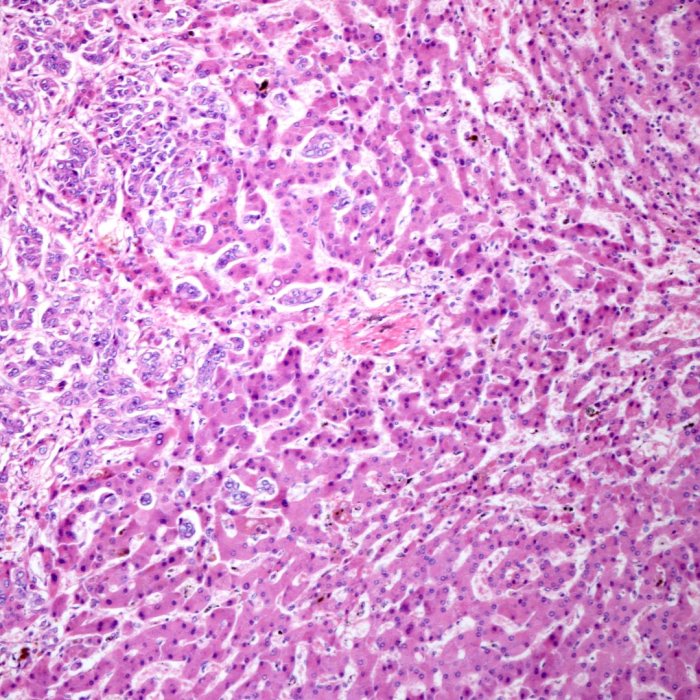
Pancreatic cancer has a propensity for invasion. Unlike many other cancers that are generally circumscribed, pancreatic tumors are very invasive and can infiltrate the surrounding structures and even the vasculature rather quickly—this can occur very early in the course of the disease itself, subsequently making treatment even more complicated.
Understanding Vascular Invasion
Vascular invasion refers to the infiltration of tumors in pancreatic cancer into adjacent blood vessels. The SMV, SMA, hepatic artery, portal vein, and jejunal branches represent vessels commonly involved by encroachment. Vascular involvement by the tumor provides very difficult management for both the surgeon and the oncologist.
The infiltration of one of the major blood vessels invaded into the pancreas makes it potentially very susceptible to such invasion. Therefore, the SMV, portal vein, which drain intestines blood, and drain it to the liver, the hepatic artery to the liver, and the superior mesenteric artery to intestines are also often around. Such relations, in which a tumor invades the bed of these vessels, can therefore lead to disturbances in blood flow and further, in the portal hypertension, intestinal ischemia, and failure of liver functions.
Vascular invasion is an important factor when determining the stage of pancreatic cancer and, in so doing, the likelihood of surgical intervention. Vascular invasion classically, biologically, has always been the determinant for unresectable cancer: an absolute no for surgery. However, with the new insights into the actual pathology of vascular invasion and the arrival of better surgical techniques, that age-old adage is being challenged. This gives some hope to patients like Sarah.
Vascular invasion in pancreatic cancer complicates the entire treatment process with numerous challenges. Foremost is the poor probability of eliminating all the cancerous tissues through the surgical procedure, the only available treatment currently. Safe resection of all cancer tissues with the preservation of flow to major arteries and veins becomes very challenging, especially when the major blood vessels are eroded by the tumor.
Sometimes, even the portal vein, and other important veins in the liver, into which the tumours have already invaded, doing the action at the SMV arising from the tumour. The vascular resection and reconstructive procedures involve resection of a segment of the vessel involved with the tumour inside it and recreation of the vessel to allow passage of blood. This, while offering the possibility of cure in the long run, can only be conducted with very specialized surgical skills and is associated with risks such as bleeding, infection, and reconstruction.
In addition, vascular invasion is a compounding factor in several methods of treatment, including radiotherapy and chemotherapy. Tumor invasion within blood vessels can be enhanced with the use of radiation and chemotherapy, as the highly fibrotic tissue at the periphery of the blood vessels acts as a sieve to disseminating reagents. High-dose radiation therapy in attempts to treat tissue close to large blood vessels might actually end up compromising these vital structures.
Why Infiltration of the Vasculature is a Major Critical Issue.
Infiltration of the vasculature is a crucial critical issue in patients with a diagnosis of pancreatic cancer. For a historical perspective, infiltration of the vasculature appeared to be grim with poor prognosis and very few therapeutic options. Most of the patients diagnosed with vasculature infiltration are usually labeled inoperable, and little else remains for them other than palliative care.
It was considered traditionally that after a mass has invaded big blood vessels, it is non-resectable, and hence removal of the mass is not possible by surgery. The resection of the tumor is fraught with risks and remains near impossible, with incomplete resection leading to distant metastasis of the tumor on follow-up. As a result, the group of patients with vascular invasion was often refused potentially curative surgery and remained open to a more aggressive course of the disease, with correspondingly shorter overall survival times.
During the last 2 decades, advances in imaging, surgical, and multimodal clinical approaches improved significantly, challenging this latter perception. High-powered imaging modalities such as contrast-enhanced MRI/CT scans are enhancing the accuracy of preoperative staging with growing confidence, and hence identifying those patients in whom it may be beneficial to perform vascular invasion surgery. More sophisticated techniques of surgery, like vascular resections and reconstructions, have broadened the horizon of patients who can be considered curable by resection.
Hope in the Horizon: Different Approaches of Treatment
Though this invasion challenges new hope in a patient with pancreatic cancer, new hope is rising up. In the meantime, modern surgical embodiments, for example, vascular resection and reconstruction, currently signpost versions of operations that perhaps will prove amenable to cure even in a larger number of patients. Innovation in neoadjuvant treatment, where this method applies chemotherapy or radiotherapy for non-operated cases, continues further to reduce the tumor size and the level of vascular invasion to make surgery a success in the end.
Personalized medicine has advanced wonderful opportunities for patients with pancreatic cancer. Scientists have identified specific mutations that may be associated with new therapies and treatments through the genetic make-up of the various tumors. When used in combination with traditional treatments, these therapies have great potential to be curative of the cancer in the pancreas with vascular invasion.
Clinical trials play a very essential role in the development of treatment of pancreatic cancer invading vasculature. Researches are going on with newer combinations of drugs, immunotherapies, and modern surgical techniques that will offer completely better results for patients combative to this challenging situation. Much work is pending; however, the advances that are made through this research and development will ultimately lead to better treatment, extended survival, and life.
Pancreatic cancer is a formidable foe, and the infiltration of blood vessels further exacerbates all the problems that are part and parcel of this disease. It's the same old charade for this cancer, yet for the newly diagnosed patients with this tough disease, there is a new sense of hope with these facts: because of current research, improvements in surgical methodologies, and the dedication of health attendants.
As in her case, patients with pancreatic cancer endure a very difficult moment, with so much resilience, innovation, and moving forward towards better outcomes. This is the era of learning from the disease with every moment of further refinement in better ways of treatments. For patients with pancreatic cancer and most importantly for patients with vascular invasion, the future looks optimistic. The road ahead is hard, but with each new discovery and each successful surgery, we approach a bit closer to turning the tide against this relentless disease.