Phone
+90 532 203 7931Complex Case - Multidisciplinary Approach to Treatment
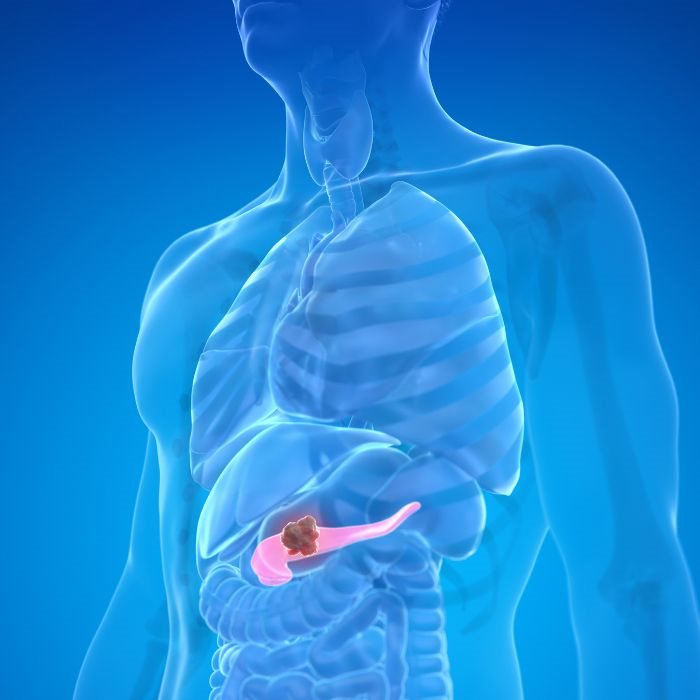
Our institute provides expert management for patients of pancreatic cancer, especially when the ailment goes over and invades critical vessels of blood supply. Traditional radiology techniques of CT scans, MRIs, and Doppler ultrasounds quite frequently suggest that these tumors are extensively invading the surrounding vascular structure, which makes them appear inoperable. Our clinical experience has taught us that all of this imaging can be quite misleading. When patients undergo surgery, we find that in about 85% of these cases, the extent of vascular invasion is much less than initially feared. It allows for surgical intervention where, before, there was absolutely none.
Our approach is based on the latest of surgical advances and deep knowledge of the biology of the tumor. We think that every patient should have a thoroughly evaluated case and that more often than not, available surgical options are there even if the imaging suggests otherwise. We work to provide new hope to patients who may have been told there was no treatment for their condition by challenging conventional thinking and looking at all possibilities. Our mission is to push the boundaries of what is possible in the care of pancreatic cancer so each patient receives a personalized plan that has the best chance of a positive outcome.
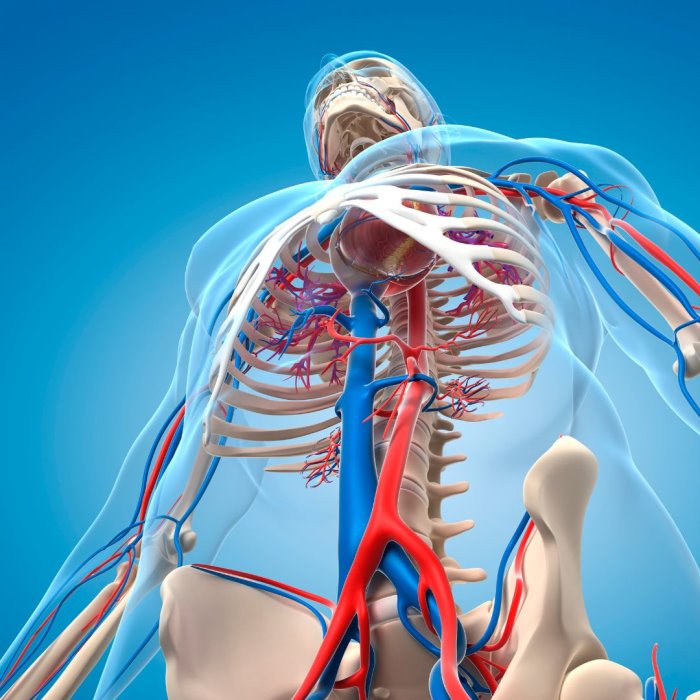
Understanding Vasculature Invasion
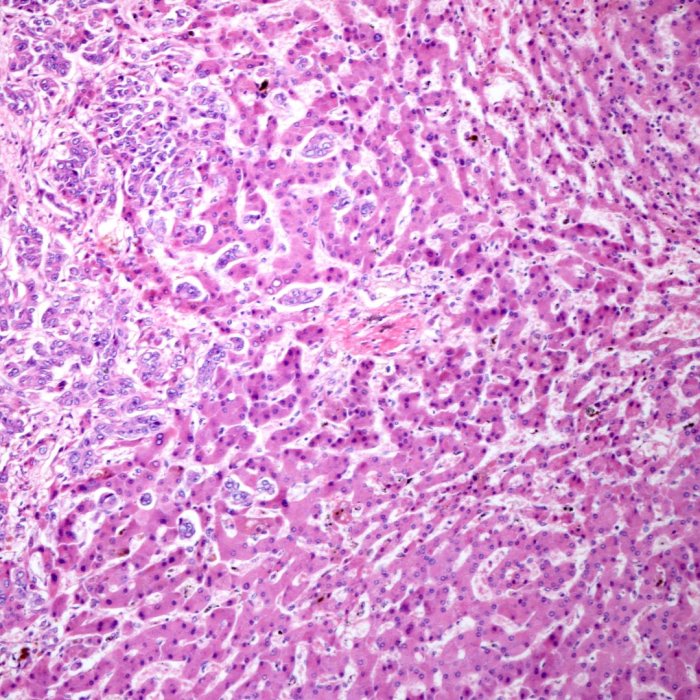
Vascular invasion in pancreatic cancer describes the extension of this tumor in the surrounding blood vessels, mainly involving the superior mesenteric vein, superior mesenteric artery, hepatic artery, portal vein, and jejunal branches. This is known to be one of the most outstanding factors against surgery. Previously, it was thought towards these cases being inoperable. However, in the current era of advanced diagnostics and surgical techniques, vascular invasion is no longer deemed to be a strong contraindication to surgery.
Our group has rich experience with these complex cases. We therefore assess every patient's treatment in depth, and by the use of advanced imaging techniques and intraoperative assessments, we try to get a clear understanding of the relationship the tumor has with the surrounding vessels. This consequently allows us to shape surgical strategy to the challenges of each case with maximal chances of good outcome and minimal risks to the patient. Attention to the problem of vascular invasion often affords us the ability to provide surgical options in which there can be meaningful chances at long-term survival.
Advanced Surgical Techniques
1. Appleby Procedure
The Appleby procedure is a specialized surgical technique in which the pancreas is removed along with parts of the implicated blood vessels, mainly when the cancer has invaded the celiac axis. This is a customized approach for a patient who has locally advanced pancreatic cancer, meaning that the tumor has extended to involve the key vascular structures. This way, we can often achieve clear surgical margins by removing those portions of the vessels that are involved and then reconstructing them. The Appleby operation is in effect a quantum advance in the treatment of pancreatic cancer—one that offers the hope of curing patients who heretofore have been deemed inoperable. From the preoperative planning to the postoperative recovery, we exercise close interaction with every patient to ensure the best possible outcome using the latest techniques and technologies that add to surgical precision and patient safety.
2. Triangle Operation
The Triangle Operation is yet another advanced form of surgery, which is mostly effective in the case of tumors located in the pancreas which have invaded into multiple vascular structures.This procedure would necessitate the resection not only of the pancreas but also of the surrounding blood vessels and tissues that are involved to present a clear margin around the tumor.
This is one of the most outrageous kinds of surgical procedures available for patients told that their cancers were inoperable because of broad vascular involvement of the cancer. Triangle Operation is a complex surgery requiring a maximum amount of knowledge and technical skills, provided by an approach towards multidisciplinary care. Here a team of surgeons, oncologists, and radiologists work together to carefully plan and execute this complex procedure: ensuring that all the different aspects of patient care are integrated and optimized. By taking an aggressive approach to tumor resection and vascular reconstruction, we can often achieve outcomes that would not be possible with less extensive surgery.This operation exemplifies our commitment to pushing the envelope of what is possible in the treatment of pancreatic cancer.
3. Vascular Reconstructions
Vascular reconstructions are a key component in the surgical treatment of pancreatic cancer, particularly in cases where tumors have invaded major blood vessels. Such reconstructions involve restoring blood flow, with repair or replacement of any affected vessels, so that vital circulations in the body are maintained alive. By confronting the vascular involvement head-on, in many instances, we will be able to remove the tumor completely while preserving the function of essential blood vessels. Our large experience in vascular reconstruction speaks to providing patients with the best possible results using the most modern techniques and materials. Our approach is to extend the boundaries of resectability, giving hope to patients who have been told that their tumors are inoperable because of vascular invasion.Vascular reconstructions can be combined with the latest techniques of tumor resection to often achieve outcomes that give a meaningful chance of long-term survival.
4. Shunt Surgery
This is a technique used in some instances for the management of the effects of vascular invasion on pancreatic cancer. A shunt surgery may be used to bypass the blood around an obstructed area of a major blood vessel, like the portal vein, caused by the tumor. This enables us to relieve the symptoms and create a more favorable environment for posterior tumor resection when extensive invasion of the surrounding vessels is present. Shunting surgery forms a very useful armamentarium in the armory in the management of complicated cases of pancreatic cancer because there is a possibility of bypassing vascular invasion yet maintaining blood flow to the vital organs.
Our team of surgeons has all the expertise in laying this new shunt by the newest techniques, so it gets laid right and functions right too.By incorporating shunt surgery as a part of our treatment strategy in these patients, resectability of the tumor can often be increased and hence the overall outcome for the patient improved.
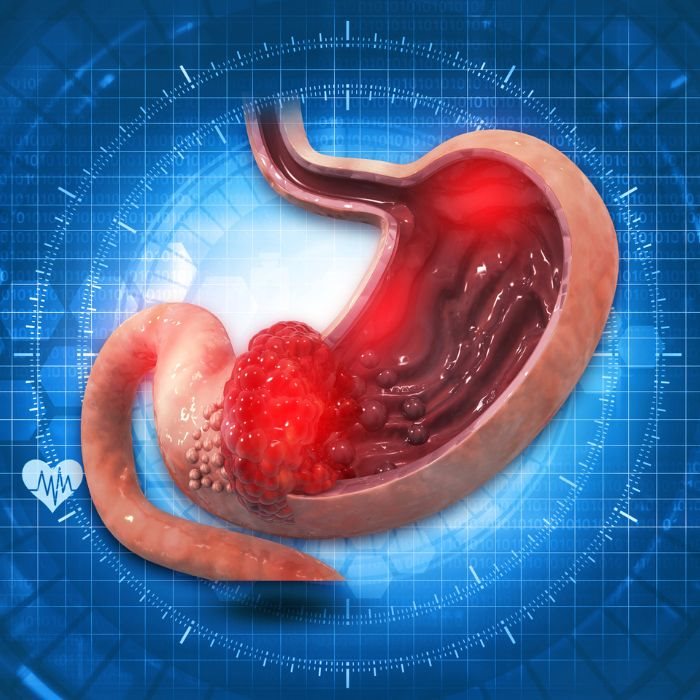
The Reality of Imaging vs. Surgical Findings
Perhaps one of the most notable problems when dealing with the treatment of pancreatic cancer is the contrast between what the radiology is showing and what the surgeon finds. Imaging studies, such as CT scans, MRIs, and Doppler ultrasounds, often indicate that pancreatic tumors have encroached on local blood vessels to a point that now makes them unresectable.
However, when we take patients to the operating room, we often find these invasions are not as extensive as was initially feared. It is roughly 15% of the incidence at which imaging reveals vascular invasion and tumor unresectability in actual clinical series. Thus, it is this rather large gap between the perception of a tumor conveyed by imaging means and true reality which constitutes the primary warrant in favor of a thorough surgical evaluation before a decision about the unresectability of a tumor is made. Our team finds this old conventional wisdom to be deeply challenged, if not refuted—though it remains widely supported in the literature—that vascular invasion and surgery cannot be compatible.
Many times, the ultimate multidisciplinary approach to care, advanced imaging techniques, and intraoperative assessments will allow a way to surgically remove tumors considered previously inoperable.This approach gives us a new lease of life, or even offers hope where before there was none, for the bleak scenario that many patients might have been otherwise facing: a hope for long-term survival.
A New Hope for Pancreatic Cancer Patients
Our center believes in giving the best, most aggressive available treatment to each patient, even if the results from the initial imaging look discouraging. We know how devastating the news that your cancer is inoperable can be; however, we know that imaging is not always the final word.
Our team is devoted to leaving no stone unturned regarding available treatment options, utilizing the most modern surgical techniques, and applying a multidisciplinary approach to patient care in providing hope where there is none. If you or someone you love has been diagnosed with pancreatic cancer with suspected vascular invasion, we encourage seeking a second opinion. Our experience reveals that many patients denied having no option for surgery actually were poor candidates for advanced surgical procedures, which afford them an opportunity to survive in the long run. We will try to push the borders of what is possible within pancreatic cancer care, and we invite you to explore the options together.