Phone
+90 532 203 7931A Patient's Story: Emily's Lifesaving Surgery
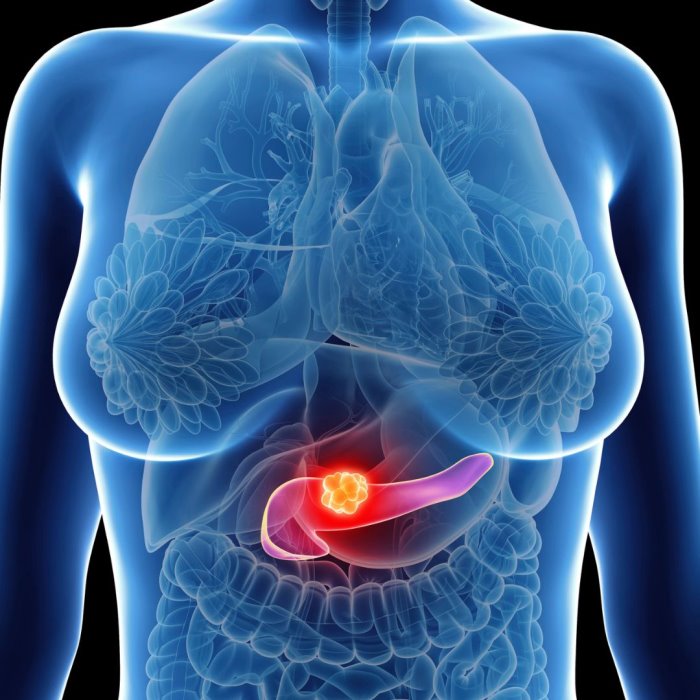
At the age of fifty-eight, Emily was a retired schoolteacher who had always been the picture of good health. However, the onset of unexplained weight loss, which consumed her, and persistent back pain made her feel as though something was awry. Subsequent testing indicated that Emily had pancreatic cancer, though in a form that was particularly hard to treat - her tumor invaded key blood vessels, making it impossible to remove in the standard surgical manner. Her physicians reviewed that state-of-the-art surgical treatments, and after much deliberation, they planned a technically advanced surgical procedure known as the Appleby procedure. All that possibility with one choice instantly changed everything—after all, she thought her life was over.
The story of Emily is an example of how advanced surgical techniques may be of help to overcome vascular invasion in pancreatic cancer. This paper focuses on two such state-of-the-art surgical techniques, the Appleby procedure and the triangle operation. We describe how they deal with tumors having vascular involvement, and how patient outcomes are improved or else have the playing field evened out.
The Appleby Procedure: Redefining Resectability
The Appleby procedure is one of the most radical surgical procedures for the patients with locally advanced pancreatic cancer, particularly in the patients when the tumors have already spread to involve the celiac axis, being one of the most important arteries that supply blood to the stomach, liver, and spleen. In the classical mode of thinking, tumors at that station were inoperable due to very hostile surrounding and being related to a colossus of critical blood vessels. The Appleby procedure, however, allows for removal of these tumors at the expense of the celiac axis while maintaining collaterals to support blood supply to the liver.
It includes the resection of the distal pancreas, spleen, and celiac axis, hence allowing physicians to achieve a complete resection of the tumor. The reason the Appleby procedure discussed above is successful is that the body adapts itself; after the removal of the celiac axis, the flow of blood to the liver is not affected since it comes from the superior mesenteric artery in enough quantities to meet up with the needs.
Although not without risks, the Appleby procedure gives highly selected patients the chance for curative surgery that would not be otherwise possible. The potential benefits of this include improved survival rates and probable complete tumor removal; hence it offers valuable options to patients with a tumor involving the celiac axis.
The Triangle Operation: Extending the Frontiers of Surgical Possibility
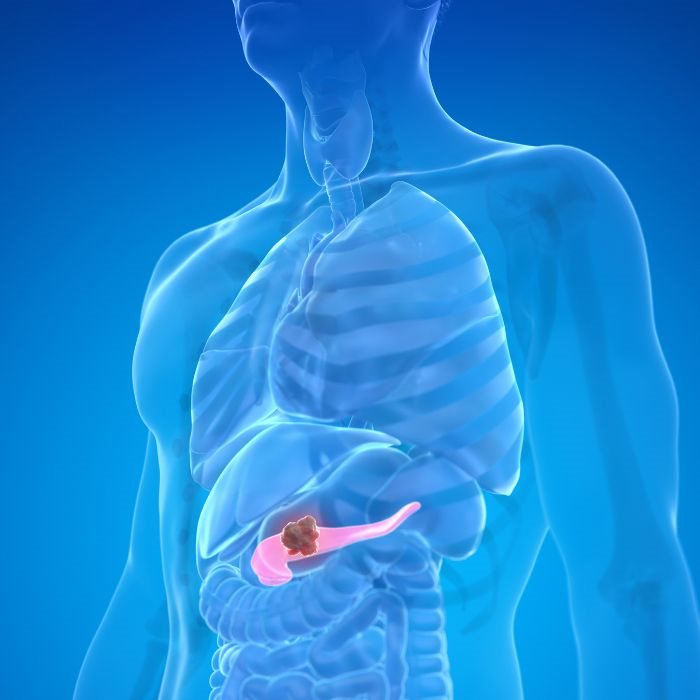
Another more advanced surgical procedure that has gained importance, treating pancreatic cancer, is the triangle operation. The triangle operation comes into the picture when a tumor invades several big blood vessels: SMA, superior mesenteric vein (SMV), and the portal vein. The surgery got its name, "triangle operation," as the surgeons aim for the triangle-shaped area involved in the procedure, which includes the pancreas, SMA, SMV, and the portal vein.
Triangle operation is a highly complicated surgery, which needs a multi-disciplinary surgical team with ability in vascular surgery, hepatobiliary as well as pancreatic surgery. The aim of the surgery is to obtain macroscopic tumor removal with a clear margin and reconstruction or preservation of the invaded vessels. It can also be vascular resection and reconstruction where the segment of the blood vessel involved is excised and replaced with a graft or re-anastomosed to re-achieve perfusion.
Triangle operation is a consideration in patients whose tumor is considered borderline resectable or locally advanced. Expansive of the resectability bracket, a great crumb of hope is given to a patient who otherwise would be having low alternatives. This can bring about a significant improvement in survival outcomes, especially when combined with neoadjuvant therapy in order to downsize the tumour before surgery.
Overcoming Vascular Involvement Challenges
Vascular involvement during the surgical management of pancreatic cancer is one of the conditions considered most difficult. Blood supply to the pancreas is through a dense network of major vessels, including the SMA, SMV, celiac axis, and portal vein. The moment a tumor develops, the invasion into the vessel, the surgical approach becomes challenging, and a complete excision is unlikely with an added risk of complications.
Advanced surgical techniques specially developed for the stated challenges include the Appleby procedure and triangle operation. Adequate planning of surgical approach by vascular resection and reconstruction techniques enables surgeons to remove tumors that have, before, been considered unresectable. These are very complex procedures that require a team of highly specialized surgeons, experienced in the management of pancreatic cancer with vascular involvement.
The outcome for these surgeries also relies on a proper preoperative assessment, which includes the use of sophisticated imaging modalities that help outline the extent of vascular invasion. This approach is combined with neoadjuvant therapy, including the use of chemotherapy or radiation in many instances to reduce the size of the tumor decreasing blood vessel involvement and making surgical resection more possible.
Improving Patient Outcomes: The Impact of Advanced Techniques
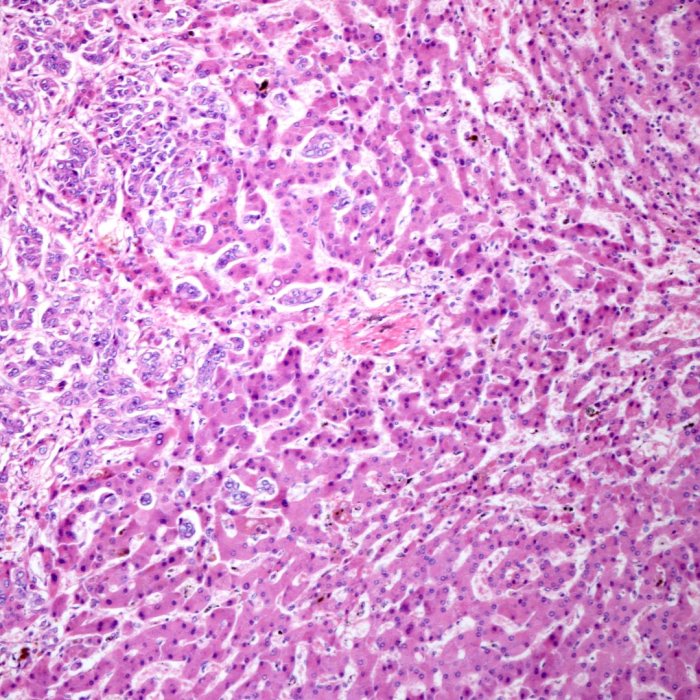
The development of advanced surgical techniques, such as the Appleby procedure and triangle operation, has dramatically impacted treatment for vascularly involved pancreatic cancer. Such procedures provide new hope for patients who were otherwise considered inoperable because those patients then have the possibility of complete resection of the tumor and better survival.
Extended survival times can be accomplished with advanced techniques. Better results were found in patients who had Appleby procedure or triangle operation, and also other studies proved that patients fared much better than those who received only non-surgical treatment. A complete resection of the tumor even with vascular involvement will allow improving better survival rates.
Besides increasing survival, these procedures may enhance the quality of life for patients with a reduced tumor burden and alleviated symptoms from pressure by the tumor on surrounding structures. For patients like Emily, in whom the prognosis was very poor, such advanced surgical options may present an opportunity for a new beginning.
The Future of Pancreatic Cancer Surgery: Innovation and Hope
With the advance in surgical techniques, it is known where the future for treatment in pancreatic cancer patients is bleak. Procedures such as the Appleby operation and the triangle operation are just some of the new techniques that are further expanding these boundaries, giving alternative options for surgery in complex and challenging tumors. This is the result of continued research, specialist collaboration, and dedication to the best possible patient outcomes.
Looking forward, new technologies into these advanced procedures further include robotic surgery and intraoperative imaging. Personalized medicine will play an increasing role in the management of pancreatic cancer with respect to surgical decision-making.
For both the patient and the clinician, the message is clear: even against the specter of vascular involvement, all hope is not lost. Advanced surgical techniques have brought new opportunities for treatment, revised traditional concepts of resectability, and have become the light at the end of the tunnel for those fighting pancreatic cancer.
Conclusion: Cutting Through the Challenges with Advanced Surgery
Pancreatic cancer with vascular involvement poses one of the greatest dilemmas in the treatment of cancer. However, modern surgical advancements, which include the Appleby procedure and the triangle operation, have ripped through minefields and are proving to be the beacon of hope for patients' survival. These procedures have made it possible to resect tumors with vascular involvement and, as such, have expanded what is considered resectable.
In these new surgeries, patients like Emily, who in the past had less choice, the implementation of these surgeries allows for a hopeful way forward, full of possibility. The more surgical advancement comes to the fore, the brighter the outlook for pancreatic cancer treatment in the future, thus lending a new ray of hope to patients and their families.