Phone
+90 532 203 7931Multidiscipline Management of Bile Duct Cancer
Cholangiocarcinoma, or bile duct cancer, is a highly malignant, infrequent tumor arising from bile ducts both within and outside the liver, being situated in a position so peculiarly awkward that not only is it often diagnosed at a rather late stage, but it can run a rapidly progressive course. Management and Treatment of cholangiocarcinoma: Cholangiocarcinoma is managed and treated with various advanced medical modalities. A very patient-oriented approach has been kept in mind while managing the disease. A multi-disciplinary team works out a personalized treatment plan keeping in view the best outcome in every patient.
The management of cancers of the bile duct demands deep understanding; for example, the dissemination of a tumor and infiltration into surrounding organs and structures. There has been a need to emphasis preciseness in care with highly sophisticated mixes of the latest state-of-the-art imaging, sophisticated surgery, and novel therapies.
Whether it is diagnosed at most latent or at the most critical stages, this is our pledge-to lead the patients smoothly and with empathy through diagnosis and treatment and into survivorship.
Understanding Cholangiocarcinoma
It is further subclassified according to the site within the bile ducts at which the cholangiocarcinoma develops: intrahepatic, perihilar, and distal. Each of these variants carries special challenges with respect to diagnosis and treatment planning, since tumor location impacts both choices of surgical options and other general management options.
Intrahepatic cholangiocarcinoma arises intrahepatically and tends to require liver resection for treatment. Most proximal, most perihilar, and most distal cholangiocarcinomas require reconstruction of the bile duct, and can be aided by liver transplantation.
Bile duct cancers are so nonspecific in their symptoms; thus, they are quite difficult to diagnose in the early stage. Most of the patients come with jaundice, unexplained weight loss, and abdominal pain.
These symptoms are nonspecific and almost invariably appear late; hence, the importance of multidisciplinary care of specialties. Thus, our oncologists work together with radiologists, gastroenterologists, and pathologists to stage properly and arrive at the best course of action a patient's condition deserves.
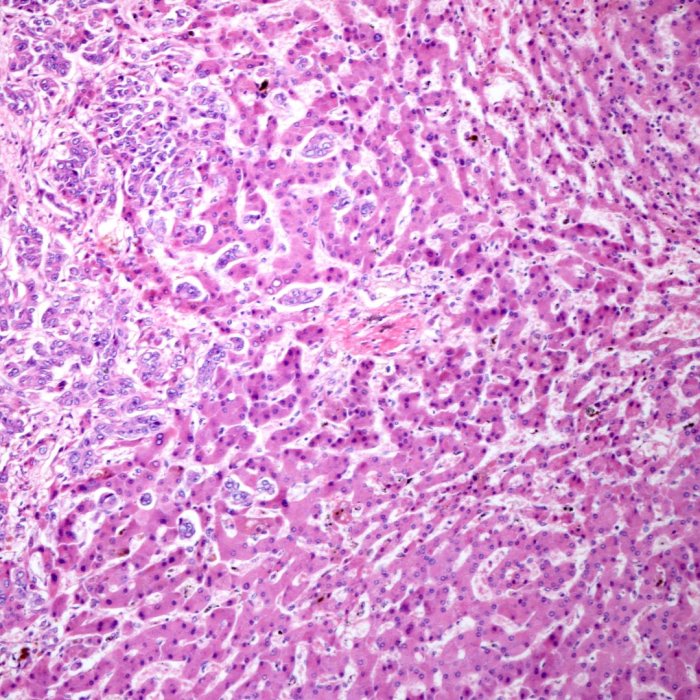
Advanced Diagnostic Techniques Indeed, correct diagnosis is the backbone of any effective treatment; similarly, it is the case in cholangiocarcinoma.
These are advanced imaging tests, including but not limited to MRI, MRCP, and PET, along with new modalities in the field of endoscopy. These studies can outline the exact site and extent of the tumor with great fidelity and thus provide a detailed roadmap for surgical planning. This enables very early and precise diagnosis, informing proper options for treatment and thus a great enhancement in general outcomes for the patient. After proper staging of the cancer, depending on the general condition of health and nature of the tumor, as a team, we recommend what is for the best: whether surgical methods alone, chemotherapy, and radiation, or all those put together-we always keep the patient in mind to ensure that symptoms are managed and side effects minimized in the treatment for the quality of life to remain optimum.
Advanced Surgical Techniques
Liver Resection
The standard of care for intrahepatic cholangiocarcinoma in general has remained surgical resection of the liver. One surgical option is the resection of the tumor, together with a margin of normal cells around it, in an effort to remove all malignant cells. The extent of the liver to be resected depends on tumor size and location and where it lies in relation to vital structures. It is sometimes enough with partial hepatectomy, but other conditions require the removal of larger portions of the liver.
These were all performed under active consultation with radiologists and hepatologists. Each one of them was designed by the surgical team in a way that would carefully preserve enough normal liver tissues that would support normal liver function. Success in the performance of liver resection in cholangiocarcinoma depends on extremely cautious preoperative and follow-up care. We further follow up on the closest monitoring of postoperative liver function and consider comprehensive support in the rehabilitation of the patient. Using a modern surgical approach, we tend to have as precise treatment planning as possible to enable us to reduce the possibility of risks and enhance postoperative recovery, hence ensuring a better long-term prognosis.
Resection of the Bile Duct with Reconstruction
Resection of the pathological part of the extrahepatic bile duct is a surgical treatment for a perihilar or distal cholangiocarcinoma; this is followed by the anatomic restoration through anastomosis of the bile ducts. Such extensive Whipple resection because of proximity to the tumor may involve the removal of adjacent tissues and organs, portions of the liver, pancreas, or small intestine. Reconstruction of the bile duct is performed either with the residuals of healthy tissue or with a portion of the small intestine.
Actually, this is very complex surgery because tumor removal needs combined input from gastroenterologists, oncologists, and intervention radiologists-this is one of those types of collaborations that minimize the possibility of complications at the cost of the digestive function of a patient. We are ready to conduct surgery planning and surgeries whereby our management ensures quality that shall finally enable restoration of natural bile flow and thereby guarantee improvement in the quality of a patient's life.
Liver Transplantation
Liver transplantation may thus be a potentially curative option for this highly selected subgroup of patients with unresectable perihilar cholangiocarcinoma. Actually, this is a rather complicated procedure whereby the whole diseased liver is replaced by a healthy donor liver. Liver transplantation can therefore afford substantial survival benefit in such patients, mainly those receiving neoadjuvant therapies to shrink the tumor before surgery. This is a rather intensive process of transplantation, considering that it requires detailed assessments regarding general health in the patient, tumor burden, and response to prior treatments. The enthusiastic transplant team will take the patient through all that, from initial evaluation and listing for a donor liver to post-transplant follow-up. Liver transplantation has, however, been proved to act like a lease of life in such patients where indicated and feasible, thus offering hope when earlier the tumor had been considered inoperable.
Symptom Relief Surgery
Symptom relief surgery is conducted when no curative surgery is contemplated. This enhances the quality of life by alleviation of symptoms. Those that may improve include obstruction of the bile ducts, reduction of jaundice, pain, and indigestion. Symptoms can be relieved either by stenting or bypass surgery that routes the bile around the tumor area-which has the aim of alleviating such symptoms and allowing the patient to live comfortably. Comfort and palliation remain an integral part of our services, though a symptom management team is devoted to working hand in hand with us in the effort to meet the physical and emotional needs of the patients. It follows, therefore, that when the disease is far advanced to alter the outcome, attention shifts to the comfort and dignity of the patient and family.
Multidisciplinary Care for Optimal Outcomes
Cholangiocarcinoma is one of the most complex tumors to manage; such treatment requires skillful coordination. Several specialists from our facility take part in contributing input on the development of an individualized treatment plan, including surgery, oncology, radiology, gastroenterology, and pathology for taking care of the patients. That is, there are regular case discussions so that management for the patient is made to suit each and every one of them for the optimization of outcomes and delivery of contemporary treatments. Bringing so many specialists together really does allow us to offer a truly comprehensive system of care for patients suffering from bile duct cancer. We will guide our patients through every stage-from initial consultation to long-term follow-up. Our pledge to the treatment of cholangiocarcinoma is a commitment to patient-oriented service for the best probability of improved outcomes with enhancement of quality of life.
Hope for Patients with Bile Duct Cancer The diagnosis of cholangiocarcinoma can be overwhelming; you are not alone. Our people are deeply committed to treating each patient with courtesy and respect. We incorporate state-of-the-art surgery, new therapies, and whole-person approaches into the care of each individual. Whether it be a new diagnosis, a recurrence, or an advanced-stage diagnosis, we are going to go through every possible option in finding a treatment approach. Aggressive yet compassionate care is the philosophy on which many of our guiding principles embark. Even when the outlook is grim, we hope. We'd be happy to explain everything from diagnosis to explaining all the various lines of treatment. We go through all steps on this journey that takes support, expertise, and a serious commitment to well-being.