The Connection Between Genetics and Oncology Surgery
Surgery in oncology has fast moved, especially with the integration of genetics into cancer treatments. Therein lies a new understanding of tumor genetics, taking surgery in oncology to where treatments are revolutionized by being far more personalized and effective. In recent years, genetics combined with surgical oncology into new pathways toward targeting cancers with greater precision and effect.
They, therefore, are able to assess and treat patients based on the specific nature of the tumor. Additionally, the genetic mutation and its expression can empower the doctors further to predict what growth pattern the tumors may take and whether certain treatments could have any recourse upon their systems or not. Thus, it becomes almost a highly individualized approach in which maximum effectiveness of the surgical modalities is achieved with minimal side effects.
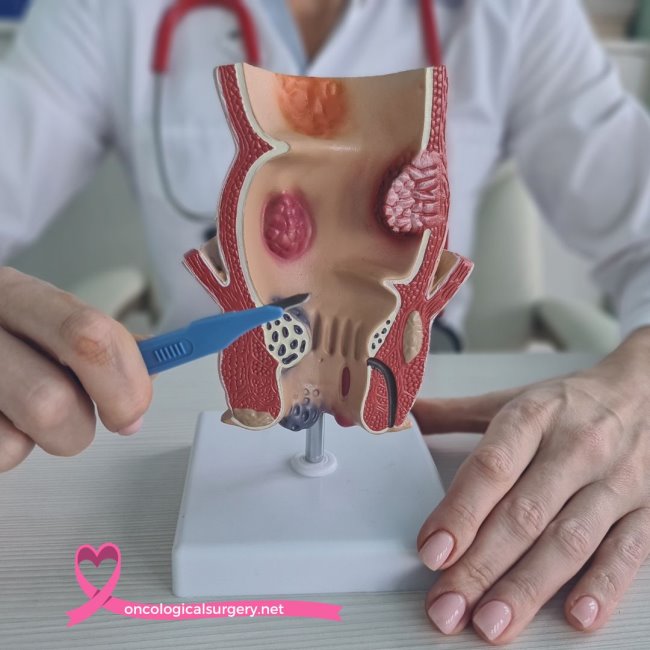
Colon Cancer Treatment Genetics
Colon cancer is one of the most common cancers in the world. Genetics also plays a crucial role in its causation and management. A few genetic mutations have been established to increase the predisposition to colon cancer, and thus genetic screening can label colon cancer as part of the early detection and preventive strategy. The genetic profile of a colon tumor instructs surgeons about the correct colon cancer treatment that should be considered when it comes to treatment. For example, specific mutations may indicate a recurrence and thereby define whether supplementary therapies must be incorporated or left out along with surgical resection.
Genetics and Improvements in Pancreatic Cancer Treatment
Pancreatic cancer is one of the least responsive tumors due to its aggressiveness and late stage of diagnosis; however, insights from genetic research have indicated potential therapeutic targets. Through such genetic alteration unique for pancreatic tumors, targeted treatments will be made possible and survival rates will be improved. END Surgical intervention remains the most important curative forms of treatment for pancreatic cancer. Genetic information can provide additional information concerning the adequacy of surgery needed and may predict better which patients will benefit from surgical resection. Finally, genetic markers are also linked to susceptibility to certain chemotherapies and may further help in providing complete treatment planning.
Genetic Influence in the Treatment of Stomach
Cancer Stomach cancer, also known as gastric cancer, results from a very complicated genetic predisposition. Yes, due to specific alterations, one may be susceptible to that kind of cancer. Genetic testing will therefore spot such susceptibility long in advance for marshaling a proactive intervention and follow-up.
It may also aid in surgical decision-making in the management of stomach cancer. For instance, hereditary diffuse gastric cancer caused by mutations in the gene CDH1 may warrant a total gastrectomy even when there are no cancers. Awareness of such genetic predisposition ensures that the most appropriate and probably life-saving surgical intervention is given to the patient.
Genetic Factors in the Management of Thyroid Cancer
It is realized that in medullary thyroid carcinoma, especially that associated with MEN2 syndromes, genetic predisposition plays a very important role in thyroid cancer. Hence, genetic testing for the RET proto-oncogene mutations becomes obligatory since treatment as well as recommendations about family screening depends on the results. These genetic mutations have enlightened surgeons who will be able to execute the most suitable treatment for thyroid cancer. In the event of inherited cases, preventive surgical intervention through the removal of the thyroid gland before the disease sets in is recommended. Better prognosis and low risks of recurrence of the disease are assured through genetic-based surgical planning.
The Oncologist Role in Genetic-Based Cancer Treatment
Oncologists are at a very pivotal position where genetics is woven into the fabric of cancer care: they assess genetic risk factors, interpret genetic testing results, and integrate such information into treatment decisions. Expertise ensures that patients receive personalized therapies tailored to their specific cancer type and genetic profile . [/end Hence, the doctors work in collaboration with the genetic counsellors and surgeons to develop an appropriate treatment plan for the patient. Indeed, collaboration achieves the optimization of whatever intervention, hence beneficial to the patient. Such an act underlines the importance of genetics in contemporary oncology practice.
Benefits of Consulting a Private Oncologist
Genetic testing has now become an integral part of surgery in oncology. Specific mutations, as identified through tests, enable surgeons to adapt the approach according to each particular individual. For this purpose, genetic markers will indicate whether less invasive surgery is required for a patient or if there is more of a need for a radical approach in the line of treatment. This level of accuracy in surgical planning prevents excessive tissue loss and therefore retains function, improving quality of life following surgery. In addition, if the underlying cause of a genetic mutation is understood, then surveillance strategies can be developed, such that any recurrence can be caught early, when it is most treatable.
Ethical Considerations in Genetic-Based Oncology Treatment
While genetics gives great advantages in oncology, it also raises some ethical problems. Genetic privacy, risk of discrimination, and psychological consequences of genetic information are things that need to be handled separately. The role of the oncologist is to explain to the patient the consequences of such a test. This involves the cornerstones of any ethical care-informed consent and genetic counseling. It is important to let him know how his genetic information is going to be used and what that would imply to him and his family. On the other hand, this is weighed against the benefits of personalized treatment, an important aspect of modern oncology. Future of Genetics in Oncology Surgery Genetic integration into oncology surgery remains an evolving domain full of immense possibility. Advances in genomic sequencing and bioinformatics now determine more precise definitions of cancer-driving mutations. Such progress promises even more personalized and effective surgical interventions in the near future. For example, studies into technologies such as CRISPR in the field of gene editing could work out novel modes of treatment or even complete prevention for specific types of cancers. With further understanding of cancer genetics, oncology surgery would change accordingly and constantly, offering better hope for outcomes and survival rates.
Genetics and oncology surgery are great strides forward in treating the cancer disease. Genetic information on the character of a disease will, in the future, enable the oncologist and surgeon to provide more personalized and more effective management, addressing the needs of a particular patient with his or her own particular genetic background. This not only raises the bar on treatments that are effective against a wide range of cancers, including but not limited to colon, pancreatic, and stomach cancers, down to thyroid cancer.
Patients should share information regarding genetic testing and treatment with their healthcare providers. This is done by consulting an oncologist or finding a private oncologist to share the genetic aspect in care.